📌 Key Takeaways
Morning grogginess from non-controlled sleep medications usually signals a timing issue, not the wrong prescription—simple adjustments within your first week resolve most discomfort.
- Timing Beats Dose Changes: Shifting your medication 15–30 minutes earlier often eliminates morning fog without changing your prescription strength.
- Track With a Clarity Score: Rating your morning alertness daily (1–10 scale) reveals patterns faster than vague impressions alone.
- Apply the Three-Item Avoid List: Cutting alcohol within 4 hours of dosing, caffeine after 2 p.m., and screens before bed amplifies medication effectiveness.
- Know When to Check In: Persistent sedation beyond 7 days, repeated falls, mood changes, or rash warrant clinician contact, not continued self-adjustment.
- Consistency Stabilizes Your System: Locking a 30-minute dosing window gives your brain the predictable anchor it needs to adapt within days.
Most mild effects vanish when timing, habits, and tracking align—patience through week one pays off.
Adults seeking faster sleep improvement with non-addictive prescriptions will gain confidence managing their adjustment period, preparing them for the detailed medication guidance and step-by-step playbook that follows.
You took your first dose last night. Now it’s 7 a.m., and your head feels wrapped in cotton.
Picture this: you have a presentation at 10, your coffee isn’t cutting through the fog, and you’re already second-guessing whether this medication was a mistake. Your partner notices you moving slowly and asks if you’re feeling okay. The doubt creeps in.
A side effect is an expected, non-target effect a medication can cause while it helps with sleep. With non-controlled sleep medications, that often looks like a little extra sedation or dryness while the body adjusts, especially in the first week or two.
Here’s the reassuring truth most people discover within their first week: that groggy morning feeling usually isn’t a sign that the medication is wrong for you. Think of it like getting new glasses—the prescription may be right, but the first few days can feel slightly “off” until the brain recalibrates. Within several nights, as your timing stabilizes and your body adjusts, most of that initial distortion fades.
This guide walks you through a simple system for managing common, mild side effects:
- Lock in a consistent dosing window
- Track your mornings with a 1–10 clarity score
- Apply a short “avoid list”
- Know when to check in with your clinician versus when to give your body another night to adjust
Most mild effects settle within days when you follow this approach.
Ready to start treatment? Begin your sleep treatment plan or explore which medications we offer.
What Counts as a “Common, Mild” Side Effect?
Understanding the difference between temporary adjustment symptoms and situations that need attention helps you respond appropriately and avoid unnecessary worry.
Mild effects are uncomfortable but manageable: symptoms that do not threaten safety, do not rapidly worsen, and do not interfere with basic functioning. These are transient symptoms that typically appear in the first several nights and resolve as your body adapts to the medication. They respond well to simple timing adjustments or minor habit changes.
Some situations require prompt attention: effects that persist beyond the initial adjustment period, worsen over time, or indicate you need to reconnect with your clinician.
Across the three main non-controlled sleep medications we prescribe, certain mild effects appear most frequently during the adjustment period:
Trazodone commonly causes morning drowsiness that lingers into the first hour after waking, along with occasional dizziness when standing up quickly. Some people notice mild headaches or a slightly dry mouth. According to MedlinePlus, these effects are well-documented and typically diminish with continued use.
Hydroxyzine tends to produce noticeable sedation, which is actually its intended effect, plus dry mouth in some users. The sedation usually feels most pronounced during the first few nights. The MedlinePlus hydroxyzine guide notes that drowsiness is the most commonly reported effect.
Clonidine may cause dry mouth, mild dizziness, fatigue, and occasionally constipation. Because clonidine also affects blood pressure, some people notice lightheadedness when transitioning from sitting to standing. These effects are detailed in clonidine prescribing information and generally improve as your body adjusts.
For a complete overview of your medication options, see our Medication Selection page.
Why Most Effects Fade as Your Timing Stabilizes
Your body operates on rhythms. When you introduce a new medication, especially one that affects sleep architecture, your system needs time to integrate it into your existing patterns. The first few nights represent a calibration period.
Think of it this way: your brain has spent years developing its current sleep-wake patterns, even if those patterns aren’t serving you well. A new safe sleeping pill shifts the balance. The initial grogginess or other mild effects often reflect your brain’s temporary confusion about the new signals it’s receiving.
By maintaining a consistent dosing window, you give your body a predictable anchor point. Within several nights, most people find their systems have adapted, and the adjustment symptoms have significantly diminished or disappeared entirely.
For deeper context on how these medications work, see How Non-Controlled Sleep Medications Work (Without Dependency).
Common Effects and Simple Fixes
This reference table covers the most frequently reported mild effects and provides straightforward responses. Keep it handy during your first week.
Symptom | Likely Cause | Tonight’s Tweak | What to Avoid | When to Check In |
|---|---|---|---|---|
Morning grogginess | Medication still active at wake time | Take dose 15–30 minutes earlier | Alcohol within 4 hours of dosing; sleeping in on weekends | Persists beyond 5–7 days despite timing adjustment |
Headache | Dehydration or sleep architecture shift | Drink 8 oz water with dose; ensure adequate hydration throughout day | Caffeine after 2 p.m.; alcohol | Severe or worsening; accompanied by vision changes |
Dry mouth | Antihistamine or alpha-agonist effect | Keep water at bedside; consider sugar-free lozenges | Mouth breathing; alcohol; excessive caffeine | Interferes with sleep; causes dental concerns |
Lightheadedness on standing | Blood pressure adjustment (especially clonidine) | Rise slowly from bed; sit at edge for 30 seconds before standing | Standing up quickly; hot showers immediately after waking | Causes falls or near-falls; accompanied by fainting |
Mild nausea | Taking medication on empty stomach | Take with small snack (crackers, banana) | Large, heavy meals close to bedtime | Vomiting; unable to keep medication down |
Vivid dreams | REM sleep rebound or medication effect | Note timing; often diminishes within first week | Screen use within 90 minutes of bed | Nightmares causing significant distress; acting out dreams physically |
The “when to check in” column represents when to reach out to your clinician through our contact page or via the patient portal. Effects in the “tonight’s tweak” category are generally safe to self-manage for several nights.
Tame Morning Grogginess With Timing, Not Bigger Doses
When morning fog persists, the instinct is often to wonder whether you need a different dose. In most cases, timing adjustments resolve the issue more effectively and more safely than dose changes.
The principle is straightforward: non-addictive sleep medications have specific durations of action. If you’re waking up groggy, the medication may still be at active levels in your system at your wake time. Moving your dose earlier gives the medication more time to clear before your alarm goes off.
The 1–10 Morning Clarity Score
Rather than relying on vague impressions, track your mornings with a simple numeric scale. Each morning, within 30 minutes of waking, rate your mental clarity from 1 to 10.
A score of 1–3 indicates significant fog: difficulty forming thoughts, strong desire to go back to sleep, feeling heavily sedated.
A score of 4–6 represents moderate grogginess: functional but not sharp, needing extra time to get going, coffee feels essential.
A score of 7–10 means good clarity: alert, able to think clearly, ready to engage with your day.
Your target is consistent scores of 7 or above. Track this alongside your dose time and bedtime for at least five nights before making adjustments. Patterns become visible quickly.
The 15–30 Minute Micro-Adjust Rule
If your Morning Clarity Score stays below 7 for three or more consecutive nights, a timing adjustment may help.
This conservative adjustment approach is widely used in sleep medicine: change timing before changing dose, and change in small steps.
If grogginess is your main issue (you feel sedated upon waking), shift your dose 15–30 minutes earlier. This gives the medication additional time to metabolize before morning.
If you’re waking too early and then feeling groggy (the medication seems to wear off prematurely, you wake at 4 a.m., then feel foggy when you get up at 7), try moving your dose 15–30 minutes later.
Make only one adjustment at a time, then hold steady for at least two nights before assessing. Your clinician can provide guidance if the micro-adjust approach isn’t producing improvement after a week.
For deeper information on timing strategies, see Timing Matters: How to Avoid Next-Day Grogginess with Non-Addictive Sleep Aids.
What to Avoid While You’re Adjusting
Three common habits can amplify side effects or undermine the medication’s effectiveness. Eliminating or modifying these during your adjustment period often makes a noticeable difference.
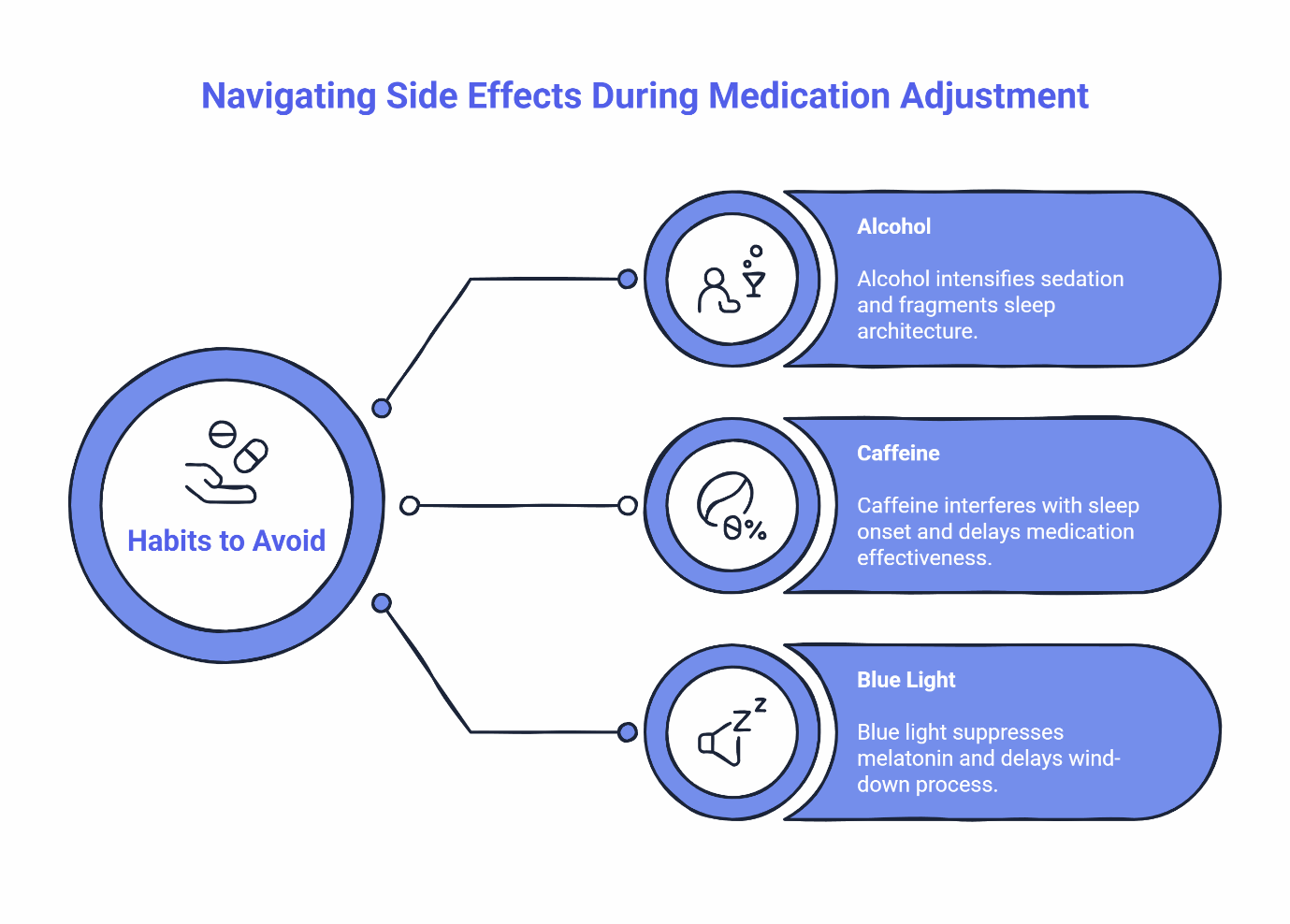
Alcohol within 3–4 hours of your dose creates problems on multiple fronts. Alcohol intensifies sedation, increasing next-day grogginess. It also fragments sleep architecture, meaning you may fall asleep easily but wake repeatedly during the night. The combination can leave you feeling worse than either substance alone. During your first two weeks, consider eliminating evening alcohol entirely. If you choose to drink, finish at least 4 hours before your planned dose time.
Caffeine after approximately 2 p.m. interferes with sleep onset. Caffeine’s half-life is roughly 5–6 hours, meaning half the caffeine from your 3 p.m. coffee is still circulating at 8 or 9 p.m. This can delay the medication’s effectiveness and cause fragmented sleep. Switch to decaf or herbal options after early afternoon.
Blue light exposure within 60–90 minutes of bed suppresses melatonin and delays your body’s natural wind-down process. Phones, tablets, computers, and televisions all emit blue light. Set a device curfew or use blue-light filtering modes if you must use screens in the evening.
These three adjustments form your “avoid list” for the first week. They’re simple but powerful. More detail on each factor is available in Non-Controlled Sleep Medications: What to Avoid to Prevent Morning Grogginess.
Important note: SleepScriptMD focuses exclusively on non-addictive sleep medication options. The platform does not prescribe benzodiazepines or Z-drugs due to their dependency risks. This approach prioritizes your long-term safety and aligns with current clinical guidance for chronic insomnia management. Learn more about our approach on the Treatments Offered page.
When to Check In With Your Clinician
Knowing when to reach out versus when to give your body more time prevents both unnecessary worry and delayed response to genuine concerns. Most adjustment symptoms resolve with the strategies in this guide, but some situations warrant a check-in with your provider.
Symptoms That Need Attention
Contact your SleepScriptMD clinician if you experience:
Persistent morning sedation that doesn’t improve after a week of timing adjustments. This may indicate the medication needs adjustment or that we should explore a different option.
Repeated dizziness or falls. Occasional mild lightheadedness when standing is common with clonidine, but repeated near-falls or actual falls require evaluation.
Palpitations or racing heart. While uncommon with these medications, this warrants prompt evaluation.
Notable mood changes. Agitation, unusual irritability, or mood shifts can occasionally occur and should be reported.
Rash or signs of allergic reaction. Contact us and discontinue the medication.
Any symptom that worsens rather than gradually improving over the first week.
These situations call for a message through the patient portal or a virtual session to reassess your treatment plan. Use our contact page to reach out.
Conditions That Need In-Person Evaluation
SleepScriptMD treats low-risk adults ages 18–65 with straightforward insomnia. Certain sleep conditions require in-person evaluation and cannot be safely managed through telehealth. If you experience any of the following, we’ll provide referral guidance:
Possible narcolepsy signs include falling asleep unexpectedly during activities like talking or driving, experiencing sudden muscle weakness during strong emotions, or feeling paralyzed when falling asleep or waking up. These symptoms require a formal sleep study.
REM Sleep Behavior Disorder (RBD) involves physically acting out dreams, including yelling, kicking, or punching during sleep. This condition requires specialized evaluation, and many sleep medications can worsen symptoms.
Restless Legs Syndrome (RLS) presents as an uncomfortable urge to move your legs at night. RLS can be linked to iron deficiency, kidney issues, or neurological conditions that require laboratory workup before treatment.
Additionally, if you’ve been told you snore heavily, gasp, or stop breathing during sleep, you may need a home sleep test to rule out obstructive sleep apnea before starting sleep medication. This ensures we’re addressing the right issue. Start with our Choose Your Sleep Quiz to assess your situation.
Eligibility note: We treat adults ages 18–65 who are not pregnant or planning pregnancy and who don’t have major medical or psychiatric conditions that could complicate treatment. If you don’t meet these criteria, we’ll guide you toward appropriate care options.
Your First 7-Night Side-Effect Playbook
This step-by-step approach gives you a structured framework for your first week. Following it consistently provides valuable data for optimizing your treatment and gives your body the stability it needs to adjust.
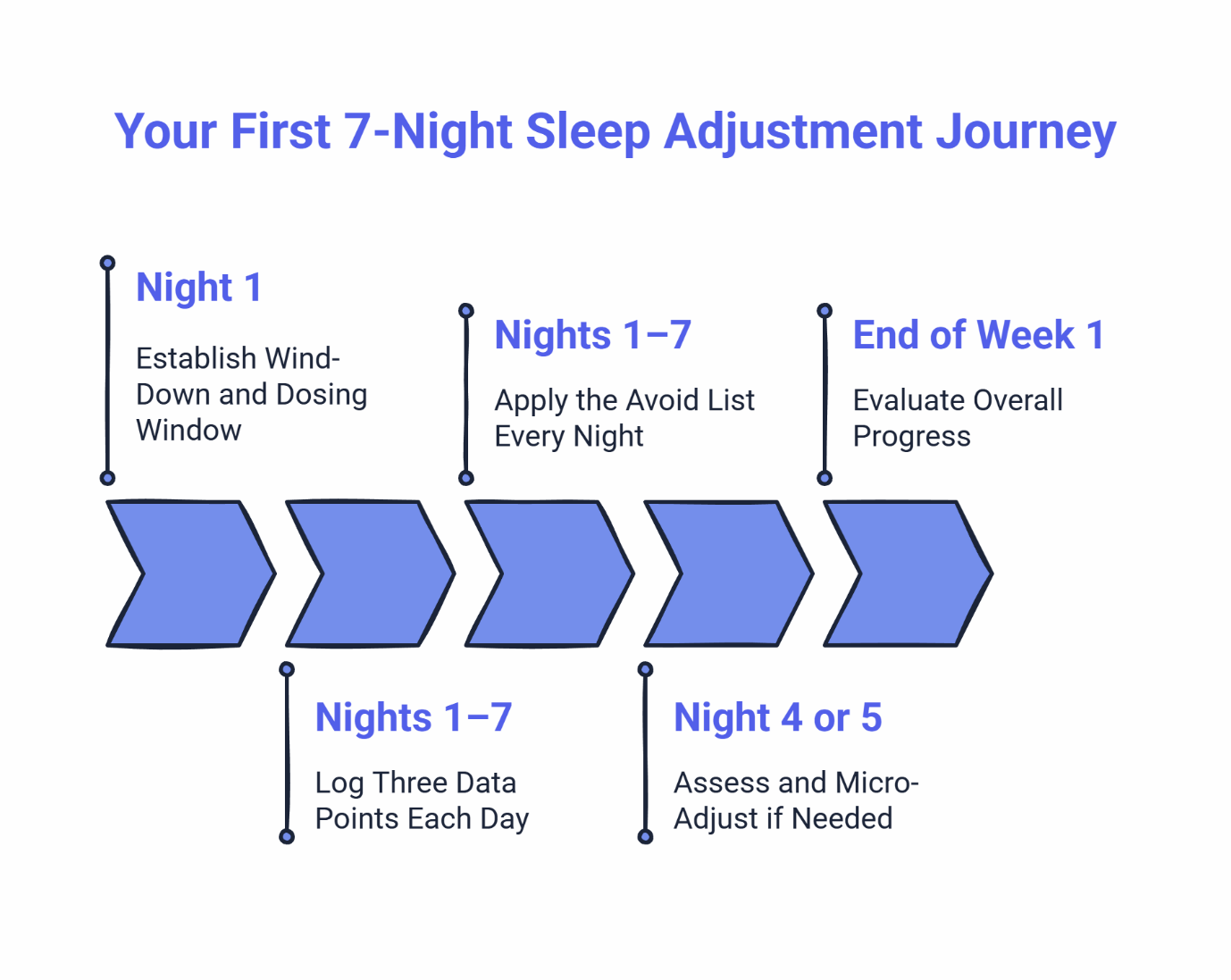
Night 1: Establish Your Wind-Down and Dosing Window
Choose a 30-minute window for your dose time and commit to it. For example, if you want to be asleep by 11 p.m., you might set your dose window at 10:00–10:30 p.m. Build a brief wind-down routine before dosing: dim lights, set out tomorrow’s clothes, do some light stretching. Consistency signals your brain that sleep is coming.
Nights 1–7: Log Three Data Points Each Day
Keep a simple log with:
- Dose time (actual, not planned)
- Bedtime (when you turned off the light)
- Morning Clarity Score (1–10, rated within 30 minutes of waking)
This doesn’t need to be elaborate. A notes app on your phone or a sticky note by your bed works fine.
Nights 1–7: Apply the Avoid List Every Night
No alcohol within 4 hours of dosing. No caffeine after 2 p.m. Screens off 60–90 minutes before bed. These three commitments give the medication its best chance to work effectively.
Night 4 or 5: Assess and Micro-Adjust if Needed
Review your Morning Clarity Scores. If they’re averaging below 7 due to grogginess, shift your dose 15–30 minutes earlier starting tonight. If you’re waking very early and then feeling groggy at your actual wake time, try 15–30 minutes later. Don’t change your dose amount without clinician guidance.
Throughout: Watch for Symptoms That Need Attention
If any of the symptoms listed in the “When to Check In” section appear, reach out to your clinician promptly rather than waiting for the full week.
End of Week 1: Evaluate Overall Progress
By night 7, most people with mild adjustment symptoms notice meaningful improvement. If your Morning Clarity Scores remain below 7, or if other symptoms persist, it’s time to connect with your clinician to discuss next steps.
For additional support, the Managing Morning Grogginess: Tips for Adjusting to a New Sleep Medication article offers expanded strategies.
How SleepScriptMD Supports Safe, Non-Addictive Treatment
The approach behind SleepScriptMD combines clinical expertise with accessibility. Understanding how the platform works helps you get the most from your care.
Physician-reviewed, AI-assisted asynchronous care means that most uncomplicated cases can receive treatment recommendations and prescriptions within the same day, with a licensed physician reviewing and approving every prescription. No prescriptions are auto-generated without physician oversight. This model provides speed and convenience while maintaining clinical safety standards.
For more complex situations, including moderate medical concerns, certain medication histories, or state-specific requirements, a brief virtual session provides direct consultation with a licensed provider. Some states require a synchronous video visit before prescribing; the platform guides you through whichever pathway applies to your situation.
Asynchronous vs. Virtual: Which Path Fits You?
Asynchronous care works well if you’re between 18 and 65, have no major medical or psychiatric conditions that could make sleep medications inappropriate, are not pregnant or planning pregnancy, and aren’t currently taking daily sleep or psychiatric medications. You complete an online assessment, a physician reviews your information, and if appropriate, a prescription is sent to your pharmacy. The AI-Assisted vs. Telehealth Appointments page details this comparison.
Virtual sessions are recommended or required if you have a more complex medical history, are taking medications that might interact with sleep aids, live in a state that requires synchronous consultation, or simply prefer direct face-to-face conversation with a provider.
Both pathways lead to the same quality of care and the same commitment to safe, non-addictive sleep med options. Current pricing information is available on our Pricing page, and the FAQ page addresses common questions about the process.
Quick Answers to Common Side-Effect Questions
How long do mild side effects last on non-controlled sleep meds?
They often lessen within several nights as your timing stabilizes. Following the first-week playbook accelerates this adjustment. If effects persist beyond 5–7 days despite timing adjustments and habit modifications, reach out to your clinician. Persistence beyond this window may indicate a need to adjust the medication choice or dosing.
Is it normal to feel groggy the first few mornings?
Yes, a brief adjustment period is common. Your brain is adapting to new sleep signals. Anchor your dosing to a fixed window and use the 15–30 minute micro-adjust approach if your Morning Clarity Score stays below 7. Most people see significant improvement within the first week.
Can I drink alcohol while taking my sleep medication?
It’s best to avoid alcohol near dosing. Alcohol intensifies sedation, fragments sleep architecture, and worsens next-day clarity. If you choose to drink, finish at least 3–4 hours before your dose time. During the first two weeks of treatment, eliminating evening alcohol entirely gives you the clearest picture of how the medication works for you.
What if I’m on SSRIs or ADHD meds?
Inform your clinician about all current medications during intake. Some combinations may require timing adjustments or closer monitoring. This is one situation where a virtual visit may be more appropriate than asynchronous care, allowing for detailed discussion.
Do I need a video visit first?
Most uncomplicated cases qualify for asynchronous care with physician review. However, some states require a brief virtual visit before prescribing, and some medical or medication histories make a synchronous consultation the appropriate approach. The intake process will guide you to the right pathway. See the Getting Started page for eligibility details.
I snore or stop breathing at night—can I still get meds?
You may need a home sleep test before prescribing to rule out obstructive sleep apnea. Treating insomnia with sedating medication when sleep apnea is present isn’t appropriate. If your history suggests possible apnea, your clinician will discuss testing options before proceeding with treatment.
Next Steps: Start Your Sleep Treatment Today
Not sure if a non-controlled sleep medication is right for your situation? Start with a quick self-assessment.
The 6-Second Sleep Check provides an instant snapshot of your sleep health. For more detailed insight, the Sleep Clarity Quiz takes about two minutes and helps identify what’s specifically impacting your rest. If you want comprehensive screening for multiple sleep issues, the Deep Sleep Profiler provides the most thorough assessment.
When you’re ready to take action, start your sleep treatment plan through the guided intake process. For complex histories or if you prefer direct consultation, you can book a virtual session with a licensed provider during the intake process.
Questions about the process? The FAQ page covers most common concerns, and the Contact page provides direct access to support.
Better sleep with clear mornings is achievable. Most mild side effects from prescription sleep aids resolve within days when you apply consistent timing, follow the avoid list, and know when to reach out for guidance. The first week requires some attention and tracking. After that, the routine becomes second nature, and restful nights become the norm rather than the exception.
Disclaimer: This content is for informational purposes only and does not constitute medical advice. Always consult with a qualified healthcare provider about your specific situation. SleepScriptMD provides care for adults ages 18–65 who meet eligibility criteria. Certain conditions require in-person evaluation and cannot be treated through telehealth.
