 Key Takeaways
Key Takeaways
Safe, non-addictive prescription sleep medications exist—and they work without the dependency risks of controlled substances.
- Non-Controlled Means Non-Addictive: Medications like trazodone, hydroxyzine, clonidine, and low-dose doxepin provide effective sleep support without creating physical dependence or tolerance.
- Matching Medication to Sleep Pattern Matters: Sleep onset issues respond best to hydroxyzine or clonidine, while sleep maintenance problems benefit from trazodone or low-dose doxepin—choosing the right option dramatically improves results.
- Timing Prevents Morning Grogginess: Taking your prescription one to two hours before desired sleep time, protecting a seven to eight hour sleep window, and avoiding alcohol eliminates most next-day fog.
- Safety Screening Protects You: Required checks for sleep apnea, narcolepsy, RBD, and significant RLS ensure medication helps rather than masks a more serious condition that needs different treatment.
- Physician Oversight Without the Wait: AI-assisted asynchronous care delivers medical review and prescription approval in minutes for straightforward cases, while complex situations receive dedicated virtual consultation.
Prepared with the right information = faster access to safe, effective sleep relief.
Adults aged 18 to 65 struggling with persistent insomnia will find practical guidance here, preparing them for the comprehensive medication options and safety protocols detailed in the article that follows.
Non-addictive sleep medications are non-controlled prescriptions—such as trazodone, low-dose doxepin, hydroxyzine, and clonidine—that can help with insomnia without creating dependence when used under a clinician’s guidance. At SleepScriptMD, we avoid benzodiazepines and Z-drugs, screen for red flags like sleep apnea, and match the right option to your sleep pattern and health history.
It’s 2 a.m. again.
You’re staring at the ceiling, wondering if there’s a safe way to finally get some rest—something that won’t leave you dependent or foggy the next morning. The good news? Safe, non-addictive prescription sleep medications exist, and they work differently than the habit-forming pills you’ve heard warnings about.
With proper medical screening and physician oversight, many adults find reliable relief through medications that improve sleep quality without the dependency risks associated with controlled substances. These prescriptions—trazodone, hydroxyzine, clonidine, and low-dose doxepin—are proven options that help you rest when it matters most.
Start your sleep treatment today, or keep reading to understand which option might fit your situation best.
The Quick Answer: What Counts as a “Non-Addictive” Sleep Medication?
When doctors talk about non-addictive sleep medications, they’re referring to prescription options that aren’t controlled substances and carry minimal risk of misuse or dependence. These are medications like trazodone (25–100 mg at bedtime), low-dose doxepin (3–6 mg), hydroxyzine (10–50 mg), and clonidine (0.05–0.2 mg)—prescriptions that were originally developed for other purposes but have proven effective for sleep when used under physician oversight.
Here’s what makes them fundamentally different from benzodiazepines or Z-drugs: they don’t bind to the same brain receptors that create physical dependence. According to the American Academy of Sleep Medicine, these non-controlled alternatives are increasingly recognized as safer first-line options for people who need pharmacological support for chronic insomnia.
These medications work through different mechanisms—some enhance natural sleep stages, others calm an overactive nervous system, and some reduce the anxiety that keeps you awake. The approach your doctor chooses depends entirely on your specific sleep pattern, medical history, and what’s actually preventing you from getting restful sleep.
For many people dealing with persistent insomnia, non-addictive sleep medications provide practical relief while you work on building sustainable sleep habits. Behavioral strategies and sleep hygiene remain important, but medication offers the immediate support that helps break the insomnia cycle while better habits take root.
Who Is—and Isn’t—a Good Fit for These Medications
Not everyone qualifies for sleep medication through a virtual platform like ours, and that’s by design. Safety comes first, which means some situations genuinely require in-person evaluation and monitoring that goes beyond what telehealth can safely provide.
You may be eligible if you:
- Are between 18 and 65 years old
- Have no major medical, mental health, or substance use conditions that could make sleep medications unsafe
- Are not pregnant and not planning to become pregnant
- Don’t have symptoms suggesting more serious sleep disorders that need specialized testing
This screening process isn’t about creating barriers—it’s about making sure you get the right level of care for your specific situation. Some sleep issues have underlying causes that medication alone won’t address, and in those cases, pointing you toward appropriate specialized care is the most responsible path forward.
When You Need In-Person Evaluation First
Certain symptoms are red flags that suggest something beyond typical insomnia, and they require a more comprehensive evaluation than a virtual platform can provide. Consider whether any of these apply to you:
□ You ever fall asleep unexpectedly during the day (while talking, driving, or during activities)
□ Your knees buckle or muscles go weak during strong emotions like laughter
□ You feel paralyzed when falling asleep or waking up
□ You physically act out dreams—yelling, kicking, or punching while asleep
These could indicate narcolepsy or REM sleep behavior disorder (RBD), conditions that require in-person sleep studies and specialized treatment. RBD, in particular, can be an early warning sign of neurological conditions and shouldn’t be treated with standard sleep medications without a proper diagnosis.
Similarly, if you experience an uncomfortable urge to move your legs at night or while resting, this could point to Restless Legs Syndrome (RLS). While sometimes benign, RLS can signal underlying issues like iron deficiency, kidney disease, or nerve damage that need to be ruled out with lab work and a thorough examination.
Important note about snoring and breathing: If you’ve been told you snore loudly, gasp for air, or stop breathing during sleep, you’ll need to complete an at-home sleep test before any sleep medication can be prescribed. Sleep apnea is incredibly common and often goes undiagnosed, but treating insomnia with medication when apnea is present can actually make things worse. The good news is that home sleep testing is straightforward, and most people can start the process within just a few days.
For any of these concerns, we’ll guide you toward the appropriate next step—whether that’s a sleep specialist, your primary care provider, or coordination with another aspect of your care.
Safety-First Options Your Doctor May Consider
When you do qualify for treatment, your provider will consider several non-addictive options based on your specific sleep pattern and medical history. Understanding how these medications work—and their trade-offs—helps you have a more informed conversation about what might work best for you.
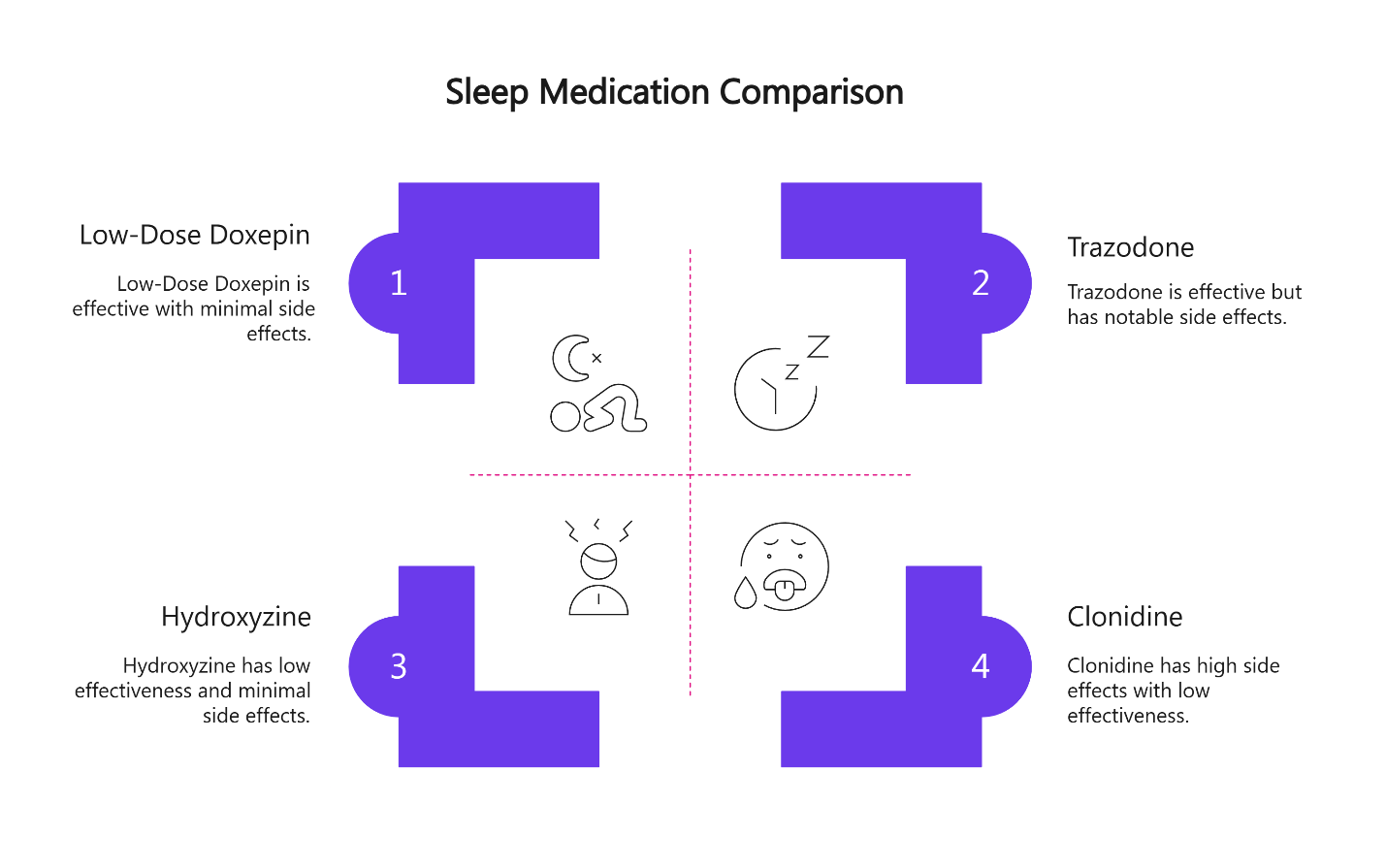
Trazodone: The Sleep Maintenance Option
Trazodone is one of the most commonly prescribed medications for insomnia, particularly for people who can fall asleep but wake up frequently during the night. Originally developed as an antidepressant, it’s used at much lower doses for sleep—typically between 25 and 100 mg taken at bedtime.
What makes trazodone particularly appealing is its potential to enhance slow-wave sleep, which is the deepest, most restorative stage of your sleep cycle. This is the sleep that leaves you feeling genuinely rested in the morning, not just technically unconscious for eight hours.
That said, roughly 10% of people report some morning grogginess, especially when first starting. This usually improves within a week or two as your body adjusts, but if it persists, adjusting the dose or timing often helps. Taking it one to two hours before you actually want to be asleep, rather than right at bedtime, can reduce that next-day fog considerably.
Trazodone does come with some rare but serious risks to be aware of. Priapism—a prolonged, painful erection—is extremely uncommon but requires immediate medical attention if it occurs. Additionally, because trazodone affects serotonin levels, combining it with other medications that increase serotonin (like certain antidepressants) can lead to serotonin syndrome, a potentially dangerous condition. Your provider will review your complete medication list to avoid this interaction.
Low-Dose Doxepin: FDA-Approved for Sleep Maintenance
Doxepin at very low doses (3 to 6 mg) is one of the few medications actually FDA-approved specifically for sleep maintenance insomnia. At these low doses, it works primarily by blocking histamine receptors, which promotes sleep without the significant side effects seen at higher antidepressant doses.
The main advantage here is targeted effectiveness. If your primary issue is waking up at 3 or 4 a.m. and being unable to fall back asleep, low-dose doxepin can be particularly helpful. It’s also a non-controlled substance with minimal abuse potential.
However, even at low doses, some people experience anticholinergic effects—dry mouth, constipation, or urinary retention. These effects become more pronounced at higher doses and can be concerning for people with glaucoma or certain other medical conditions. Starting at the lowest effective dose and maintaining consistent timing helps minimize these side effects.
Hydroxyzine: For Anxiety-Linked Insomnia
If anxiety is a significant contributor to your sleep difficulties, hydroxyzine might be the option your provider considers. Available in 10 to 50 mg doses, hydroxyzine is an antihistamine that reduces anxiety while promoting drowsiness—addressing both the racing thoughts and the sleep onset problem at once.
Because hydroxyzine is non-addictive and doesn’t create tolerance, it’s particularly appealing for people who need long-term support. It’s also remarkably affordable, as it’s been available as a generic for years.
The flip side is that hydroxyzine can cause noticeable daytime sedation for some people, especially in the first few days. If you have important commitments the next morning, it’s wise to trial it on a low-stakes day first to see how your body responds. There’s also a small risk of QT prolongation (a heart rhythm change) when combined with other medications that affect heart rhythm, so your provider will review this carefully.
Clonidine: Calming an Overactive System
Clonidine takes a different approach entirely. Originally developed to lower blood pressure, it works by reducing sympathetic nervous system activity—essentially calming your body’s “fight or flight” response. This makes it particularly helpful for people whose insomnia is driven by hyperarousal, racing thoughts, or ADHD-related sleep difficulties.
Doses for sleep are quite low, typically ranging from 0.05 to 0.2 mg at bedtime. At these doses, most people don’t experience significant blood pressure drops, but it’s still something to be aware of—particularly if you already have low blood pressure or a history of fainting when standing up quickly.
The most common side effects are dry mouth and mild fatigue. One important caution: if you’ve been taking clonidine regularly and decide to stop, you need to taper off gradually rather than stopping abruptly, as sudden discontinuation can cause rebound high blood pressure. Your provider will guide you through this process if you decide clonidine isn’t the right fit.
How to Choose: A Simple Decision Guide
Matching the right medication to your specific situation doesn’t require a medical degree—it just requires honest answers to a few straightforward questions.
If your main issue is: Difficulty falling asleep initially
Consider discussing: Hydroxyzine or clonidine (especially if anxiety or racing thoughts are involved)
If your main issue is: Waking up in the middle of the night and can’t get back to sleep
Consider discussing: Trazodone or low-dose doxepin
If your main issue is: Anxiety or racing thoughts keeping you awake
Consider discussing: Hydroxyzine or clonidine
If your main issue is: ADHD-related sleep difficulties or general hyperarousal
Consider discussing: Clonidine
This isn’t a prescription guide—it’s a framework to help you have a more focused conversation with your provider about what might work for your particular situation.
Ready to find out which option is right for you? Start your sleep treatment or see our full medication guide.
Evidence-Backed Supplements as Adjuncts
While not substitutes for prescription medications when those are needed, certain supplements can support your sleep efforts:
Melatonin is particularly helpful for circadian timing issues—like adjusting to Daylight Saving Time shifts or jet lag. For best results, take it two to four hours before your desired bedtime rather than right before bed, as it works by signaling your body’s internal clock.
Magnesium L-threonate may support relaxation and sleep quality in some people, though research is still emerging.
Always review any supplements with your clinician to avoid interactions with your medications.
Avoiding Next-Day Grogginess
That groggy, hung-over feeling the morning after taking sleep medication is one of the most common complaints, and it’s often preventable with a few strategic adjustments.
Timing matters more than most people realize. Taking your medication right as you’re getting into bed might seem logical, but many sleep medications work better when taken one to two hours before you actually want to be asleep. This gives the medication time to kick in naturally, mimicking your body’s own sleep drive rather than forcing an abrupt shutdown.
Starting with the lowest effective dose is another crucial strategy. Your provider can always increase the dose if needed, but starting high often leads to unnecessary side effects that might cause you to abandon an otherwise helpful medication prematurely.
Protect your sleep window. Keep seven to eight hours available for sleep. If you’re taking a medication at 11 p.m. but planning to wake up at 5 a.m., grogginess is almost inevitable—the medication hasn’t had enough time to clear your system.
Alcohol is a particular concern. Even a single drink can amplify the sedative effects of sleep medications unpredictably, leading to much more pronounced grogginess the next day—or even dangerous respiratory depression in some cases. It’s best to avoid alcohol entirely when taking sleep medications, or at minimum, keep several hours between drinking and taking your medication.
Finally, talk to your provider about all your medications and supplements. Interactions between sleep medications and other drugs—particularly other sedatives, certain antidepressants, or even some allergy medications—can intensify side effects or create safety concerns. A complete medication review before starting any new sleep medication is essential.
For detailed strategies on managing morning grogginess, our guide on managing morning grogginess when adjusting to new sleep medication offers practical, evidence-based tips. You can also explore timing strategies to avoid next-day grogginess for medication-specific guidance.
Making Your Medication Work Better: Simple Evening Habits
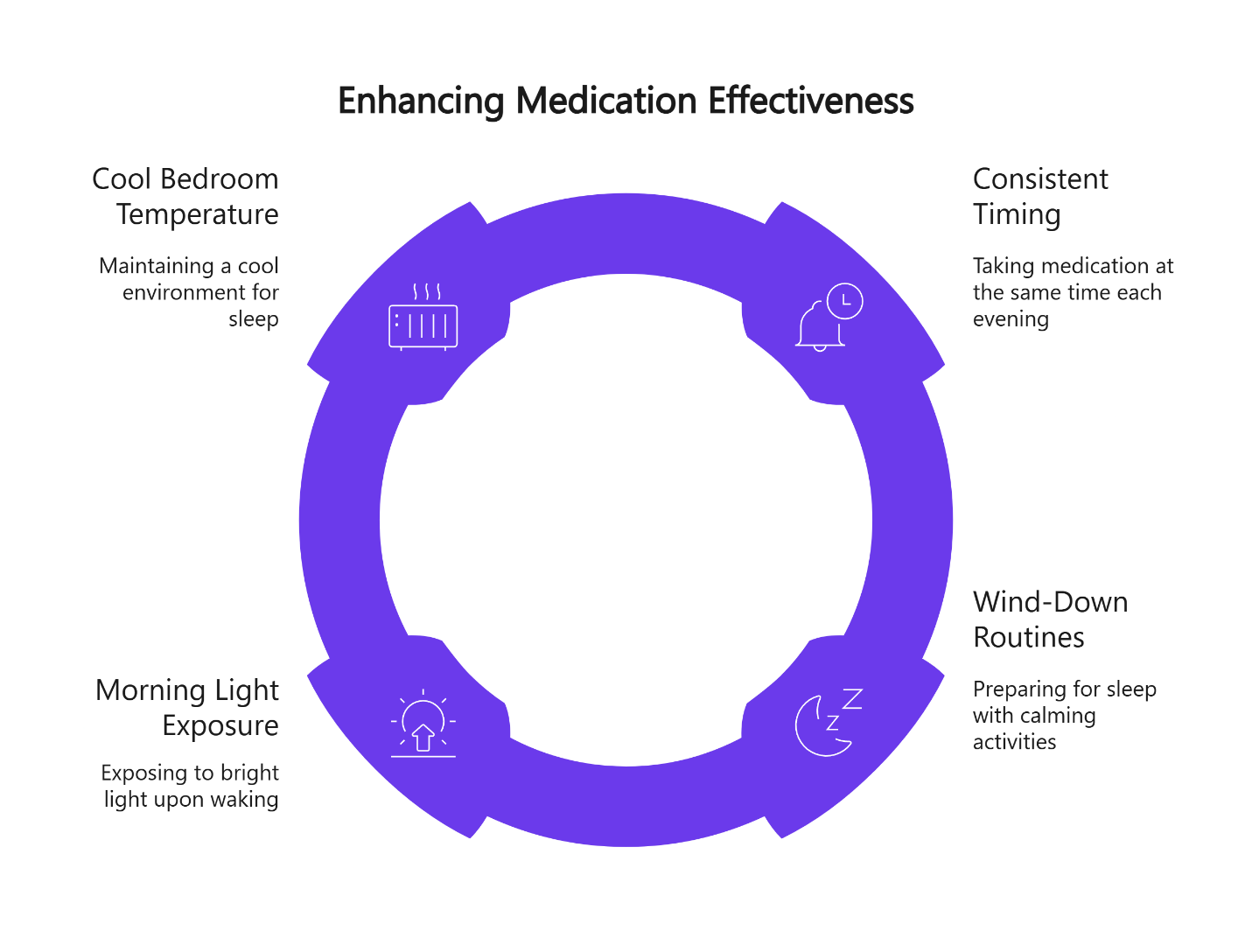
Once you have a prescription, a few practical habits can help maximize its effectiveness:
Consistent timing creates predictability. Take your medication at the same time each evening to help your body develop a reliable sleep rhythm. This consistency reinforces your natural sleep-wake cycle.
Wind-down routines support your prescription. The 30 to 60 minutes before taking your medication matter. Dim the lights, put away screens, and engage in calming activities. This signals your body that sleep is approaching and helps the medication work with your natural rhythms rather than against them.
Morning light exposure helps. Getting bright light exposure within the first hour of waking helps anchor your circadian rhythm, which makes evening medication more effective. Even 10 to 15 minutes of outdoor light during your morning routine can make a difference.
Temperature matters. Keep your bedroom cool (around 65-68°F) once you’ve taken your medication. A cooler environment supports the natural temperature drop your body needs for deep sleep.
These aren’t complicated therapy protocols—they’re practical adjustments that help your safe, non-addictive prescription deliver better results.
Navigating Seasonal Sleep Challenges
Certain times of year predictably disrupt sleep patterns, but adjusting your medication timing and routine can protect your rest:
Daylight Saving Time transitions (March and November): Rather than absorbing the full hour shift overnight, adjust your medication timing by 10 to 15 minutes per night for four to six nights before the clock change. Take your prescription slightly earlier (for spring forward) or later (for fall back) each evening. This gradual shift prevents the jet-lag-like grogginess that catches many people off guard.
Back-to-school season (August–September): Lock in a consistent wake time first, then adjust your medication timing to maintain your ideal sleep window. Take your prescription at the same time each evening—even on weekends—to prevent the schedule chaos that often comes with new routines.
Holiday stress and travel (November–December): Watch late-day caffeine, alcohol, and bright evening light, all of which can interfere with your medication’s effectiveness. If you’re traveling across time zones, consult your provider about temporarily adjusting your prescription timing to match your destination schedule.
New Year reset (January): If you’re starting a prescription in January, pair it with simple evening habits from day one. This creates a sustainable foundation that continues even if you eventually taper off medication.
Winter blues (November–February): Morning light exposure becomes even more important during darker months. Get outside within an hour of waking, even on overcast days—it helps your prescription work more effectively by reinforcing your circadian rhythm. Talk to your clinician if you notice mood changes affecting your sleep beyond what medication addresses.
Year-end deductibles (December–January): Check pharmacy pricing early if your insurance resets in January. Most of our prescribed medications are available as affordable generics, but knowing costs in advance prevents surprises when you need a refill.
Important Safety Screening Before Starting Medication
While medication can provide important relief for insomnia, some sleep issues require different interventions. That’s why proper screening before prescribing is essential.
For people dealing with snoring, witnessed pauses in breathing, or excessive daytime sleepiness despite adequate time in bed, at-home sleep apnea testing is a critical step before starting any sleep medication. Sleep apnea—where your airway repeatedly collapses during sleep—is shockingly common, affecting roughly 10-30% of adults. It causes fragmented sleep that no medication can fix, and treating insomnia with sedatives when apnea is present can actually worsen the breathing problems.
The good news is that home sleep testing has become remarkably convenient and accurate. Most people can complete the test in their own bed and get results within a few days, allowing for a clear diagnosis and appropriate treatment plan if apnea is present.
Some people also benefit from working with a therapist on sleep-focused behavioral strategies alongside their prescription. These approaches can be helpful complements to medication, though they’re not required to start treatment with us. If you’re interested in exploring behavioral strategies while on medication, ask your provider for guidance.
How SleepScriptMD Helps You Start Safely (and Fast)
Getting appropriate sleep treatment shouldn’t require weeks of waiting for appointments or navigating insurance bureaucracy. That’s the fundamental problem we set out to solve.
Our approach combines physician oversight with AI-assisted efficiency. For most people with straightforward insomnia and low-risk medical profiles, our asynchronous care path delivers treatment recommendations within minutes of completing an online assessment. A licensed physician reviews your information and approves any prescriptions—nothing is auto-generated. You’re not talking to a bot; you’re getting actual medical judgment, just delivered more efficiently than the traditional appointment model allows.
If your situation is more complex—if you have moderate medical concerns, take multiple medications, or have a psychiatric history that requires more discussion—we can schedule a brief 15 to 20 minute virtual session instead. These appointments give you direct face time with one of our providers to address your specific circumstances. Some states require a brief virtual visit before prescribing due to local telehealth regulations, so your intake process may vary depending on where you live.
The cost structure is straightforward and transparent. Our asynchronous care costs $45 for 30 days or $120 for 90 days, which covers the medical assessment and prescription approval. Virtual intake sessions are $110, and follow-up visits are $85. We often run promotional pricing to make it easier to try the service—check our website for current offers. Importantly, these fees don’t include the medication itself—you’ll pay for that at your preferred pharmacy, where most of the medications we prescribe are available as affordable generics.
Start your sleep treatment today, or compare AI-assisted vs virtual care to see which path makes the most sense for your situation. You can also see our full pricing breakdown or meet our medical team to learn more about the physicians who oversee your care.
Risk-Mitigation Guardrails We Follow
Safety protocols guide every aspect of our prescribing approach:
- We do not prescribe benzodiazepines or Z-drugs.
- Adults 18–65, not pregnant, and with a low-risk profile are eligible for our program.
- Snoring or gasping symptoms require home sleep apnea testing before any sedating medication.
- We refer patients in-person for narcolepsy, RBD, severe RLS, or complex comorbidity that exceeds telehealth’s safe scope.
Frequently Asked Questions
Are these medications habit-forming?
No. The medications we prescribe are non-controlled options that don’t create physical dependence when used as prescribed. We specifically avoid benzodiazepines and Z-drugs precisely because of their dependence risk.
Will I feel groggy the next day?
Some people experience temporary morning grogginess when first starting a sleep medication, but this usually resolves within a week or two. Adjusting the timing (taking the medication earlier in the evening) or lowering the dose typically helps. Our article on timing sleep medications to avoid next-day grogginess provides detailed guidance on minimizing this issue.
Can I use these medications if I’m pregnant or planning pregnancy?
No. Our program serves adults aged 18 to 65 who are not pregnant and not planning pregnancy. If you’re pregnant or trying to conceive, you’ll need to work with a local clinician who can provide appropriate pregnancy-safe alternatives and monitoring.
Do I need an appointment?
In most states, no. Our AI-assisted asynchronous care path doesn’t require a live appointment—you complete an assessment online and receive a treatment plan once a physician reviews your information. However, if your medical history is complex or if you prefer direct conversation with a provider, you can schedule a brief virtual visit. Some states do require a synchronous visit due to local telehealth regulations.
Is this covered by insurance?
We operate on a transparent flat-fee model rather than billing insurance, which keeps the process simple and straightforward. You pay our service fee directly, and medication costs are handled separately at your pharmacy. Many insurance plans will cover the medications themselves since they’re typically generic. You may also be able to use FSA or HSA funds for our service fees—check with your plan administrator to confirm eligibility.
Next Steps: Getting Started Is Simple
If you’re ready to explore whether non-addictive sleep medication might help your situation, you have a few straightforward options.
The fastest path is to complete our online intake form, which takes about 10 minutes and covers your medical history, current medications, and sleep patterns. If you’re eligible and your state allows asynchronous care, you could have a treatment plan and prescription sent to your pharmacy the same day in most cases.
Not sure if you’re ready for that step? Take our 2-Minute Sleep Clarity Quiz to get personalized next steps based on your specific situation. The quiz helps identify whether your sleep issues might benefit from medication, behavioral strategies, or further evaluation. You can also explore all our sleep assessment options to find the right starting point for you.
Before you start any assessment, it helps to have a few things ready: a complete list of your current medications and supplements, a clear sense of your main sleep complaint (trouble falling asleep vs. staying asleep vs. both), and any known medical conditions or allergies. If you’ve tried sleep medications in the past, knowing which ones you tried and how they worked (or didn’t) is valuable context for your provider.
You don’t have to keep living with poor sleep, wondering if there’s a safe way forward. With the right medical guidance, appropriate screening, and non-addictive options, better rest is genuinely within reach.
Start your sleep treatment now—most eligible patients receive treatment recommendations quickly, often the same day where permitted.
Disclaimer: This article is for informational purposes only and does not constitute medical advice. SleepScriptMD provides medical services to eligible patients but cannot guarantee prescription approval for all individuals. Always consult with a licensed healthcare provider about your specific medical concerns.
Our Editorial Process
All content is written by healthcare professionals with expertise in sleep medicine and psychiatry, reviewed by our medical team for accuracy, and updated regularly to reflect current clinical guidelines. We prioritize evidence-based information while maintaining accessibility for general audiences.
Author Byline
Written by The SleepScriptMD Insights Team
Medically Reviewed by David Danish, MD, Chief Psychiatric Officer
Clinical Editor: Peter Kelly, DO, Chief Medical Officer