 Key Takeaways
Key Takeaways
Reliable sleep before high-stakes days requires a plan that delivers clarity without dependency or morning fog.
- Safety-First Means Physician Review: Every prescription decision begins with contraindication screening and eligibility verification to ensure non-controlled medications are appropriate for your specific health profile.
- Continuity Over Quick Fixes: The care model emphasizes ongoing monthly subscriptions, scheduled refills, and follow-up adjustments—not short-term trials that stop after a few weeks.
- Timing Protects Morning Performance: Aligning medication intake with your natural sleep window and allowing a full 7-8 hours before wake time can help reduce next-day grogginess.
- Portal Access Between Appointments: Message your provider directly through the patient portal for timing adjustments or side-effect questions without waiting for scheduled check-ins.
- Clear Exclusions Build Trust: Certain conditions like suspected narcolepsy, REM Sleep Behavior Disorder, pregnancy, and complex medical histories require in-person evaluation and are transparently redirected to local care.
Prepared intake plus realistic timing expectations equals faster approval and steadier long-term care. Adults aged 18-65 seeking non-addictive prescription sleep solutions will find a comprehensive overview here, preparing them for the detailed consultation process that follows.
A safety-first telehealth sleep consult is a clinician-reviewed process that evaluates your sleep history, screens for risks, and—when appropriate—initiates or continues non-controlled prescription options with ongoing follow-ups and refills. At SleepScript MD, the focus is on safe, non-addictive sleep medications that help you sleep without the risk of dependency that comes with older controlled substances.
Think of it like onboarding to a trusted fitness program: you get a baseline assessment, a plan you can actually stick to, and regular check-ins to keep you on track. You need clear sleep before a high-stakes day, but you also want a durable plan that won’t leave you foggy or dependent. Here’s exactly how your first consult flows, what to have ready, and how subscriptions and refills work month to month.
The Consult at a Glance: From Intake to Ongoing Care
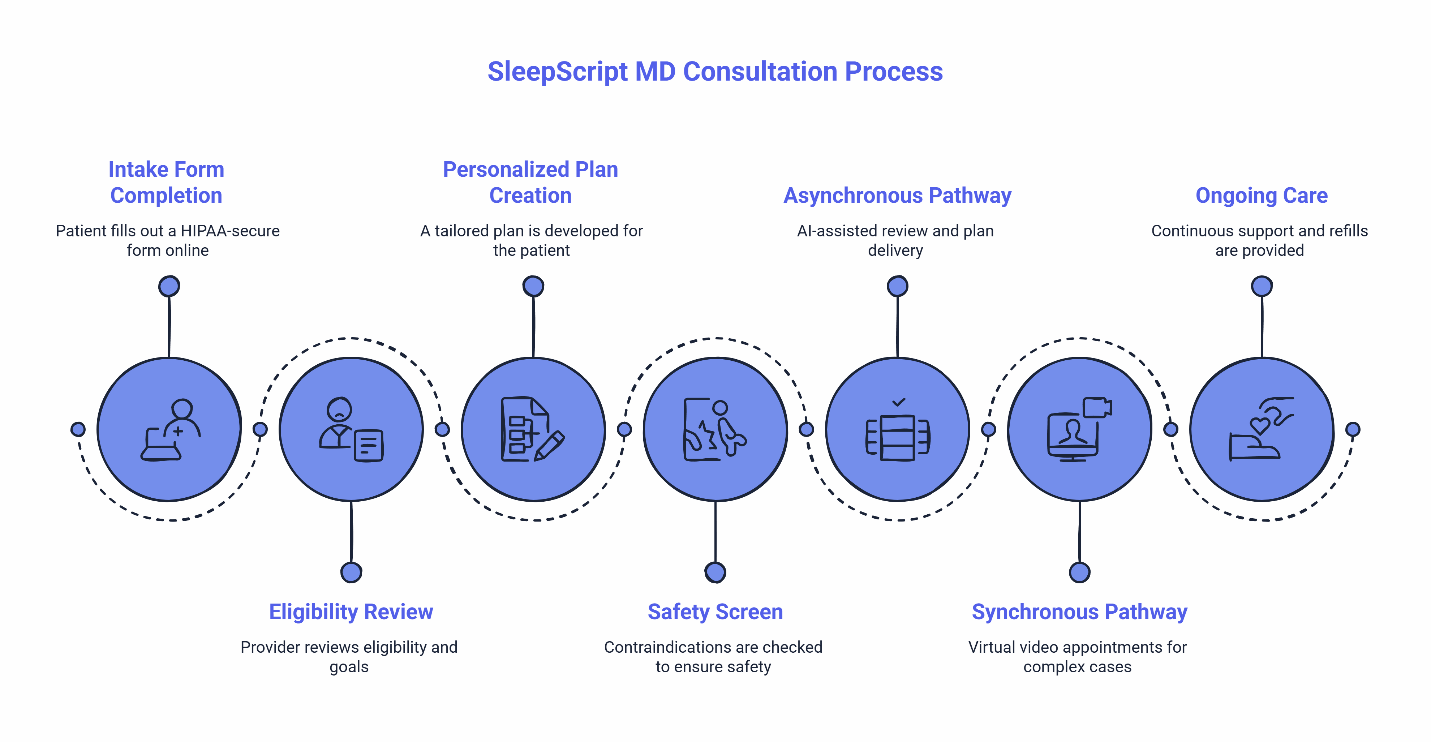
Expect a structured, clinician-guided process: intake → safety screen → tailored plan → ongoing refills and monthly follow-ups.
You complete a HIPAA-secure intake form through the platform. A licensed provider reviews your eligibility, current medications, and sleep goals. You receive a personalized plan and a clear timeline for check-ins and refills. The telehealth intake prevents inappropriate use by screening for contraindications before any prescription decisions are made.
SleepScript MD offers two pathways depending on your state and medical complexity. In most states, patients use the AI-assisted asynchronous approach, where your intake is reviewed and a plan is often provided within the same day. For those with more complex medical histories, those who prefer direct interaction, or those in states requiring synchronous care, virtual video appointments are available within five days. Both routes lead to the same outcome: a safety-first plan with ongoing clinician management and prescription sleep aids tailored to your needs.
This isn’t a two-week trial that stops abruptly. Your plan includes a clear refill cadence and scheduled follow-ups so your provider can adjust timing or dosing as your needs evolve. The goal is continuity: monthly subscription support, predictable refills, and a medication plan that works long-term.
What to Prepare Before Your Telehealth Consult
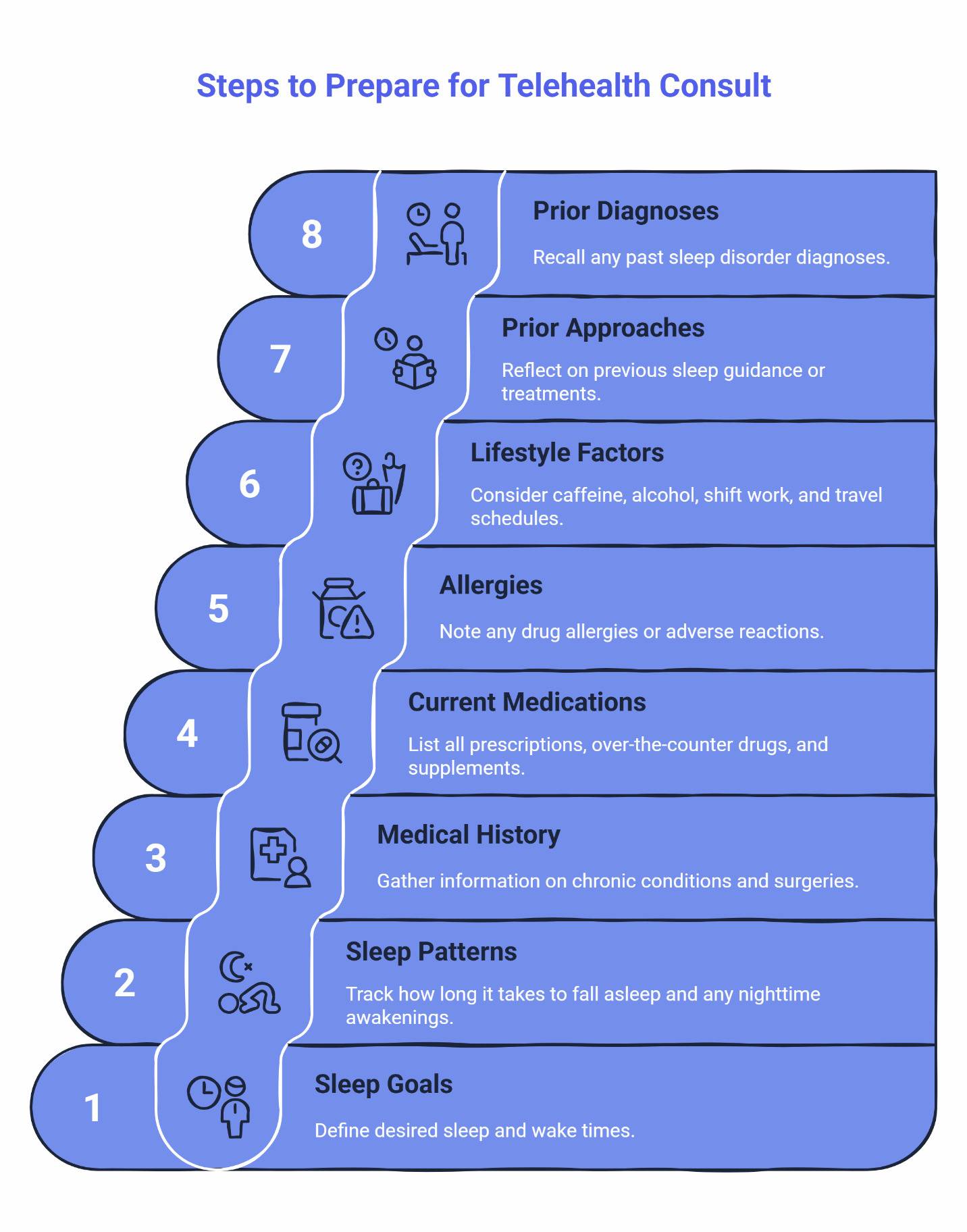
Have your sleep goals, schedule, medical history, and current medications ready. Being prepared helps your provider make better decisions and saves time.
Your Consult-Prep Checklist:
- Sleep Goals & Schedule: What time do you want to fall asleep? What time do you need to wake up?
- Current Sleep Patterns: How long does it typically take you to fall asleep? Do you wake during the night?
- Medical History: Any chronic conditions, recent surgeries, or ongoing treatments
- Current Medications: All prescriptions, over-the-counter medications, and supplements you take
- Allergies: Drug allergies or adverse reactions you’ve experienced
- Lifestyle Factors: Caffeine and alcohol timing, shift work, travel schedules
- Prior Sleep Approaches: Any previous guidance or treatments that helped or didn’t help
- Prior Sleep Diagnoses: Has anyone suggested you might have sleep apnea, restless legs, or other sleep disorders?
This checklist serves as your complete prep guide. You can save it, print it, or keep it on your phone as you fill out your intake form. For a broader understanding of the non-addictive sleep medications available through SleepScript MD, visit our treatments overview.
Safety Review: How Clinicians Personalize Your Prescription Plan
A provider screens for contraindications and customizes your medication plan based on your individual situation. The safety review isn’t about finding reasons to say no—it’s about identifying which non-controlled prescription option protects both your sleep quality and your overall health.
Contraindication screening looks at factors like age, medical conditions, psychiatric history, and current medications that might interact poorly with sleep treatments. This process ensures that non-controlled options are appropriate for your specific safety profile when they’re considered.
What We Don’t Prescribe: SleepScript MD does not prescribe benzodiazepines (like Xanax, Ativan, or Klonopin) or Z-drugs (like Ambien, Lunesta, or Sonata) due to their risk of dependency and withdrawal complications. Our focus is exclusively on safer, non-controlled alternatives.
The medication plan you receive is designed as an ongoing framework, not a quick fix. If mornings feel foggy with your current approach, timing guidance and dose adjustments can be planned over scheduled follow-ups. Adherence tracking improves outcomes by helping your provider see what’s working and what needs refinement.
Want to explore which medication might fit your sleep pattern? Visit our medication selection guide to learn more. For patient-friendly education on insomnia and evidence-based treatment approaches, the National Library of Medicine’s MedlinePlus resource and the American Academy of Sleep Medicine’s patient education portal offer comprehensive overviews.
Follow-up cadence supports refills and continuity. You’re not left wondering when to check back in or how to get your prescription renewed.
Refills, Follow-Ups, and Your Monthly Subscription
Your plan includes a clear refill cadence and monthly subscription support for continuity of care.
Automatic reminders prompt check-ins so your provider can renew medications and optimize timing. Most patients find that a monthly rhythm works well. You get a reminder, you have a quick asynchronous check-in or scheduled call, and your prescription is renewed when appropriate. This ongoing approach means you stay on your medication as long as it’s helping—not just for a brief trial period.
Between scheduled appointments, you can message your provider through the patient portal if you need timing adjustments or have questions about side effects. This ensures you’re not stuck waiting for your next appointment when something needs attention.
Returning patients have a streamlined process. The monthly subscription keeps your care continuous rather than forcing you to start from scratch each time you need support.
Billing is transparent. You see exactly what the subscription covers: ongoing provider access, prescription renewals, and the ability to adjust your plan as your sleep needs change. For complete pricing details, visit our pricing page. This model prioritizes long-term improvement over quick fixes.
Timing Guidance to Protect Next-Day Clarity
Taking your medication at the right time can help reduce next-day grogginess. This is one of the most common concerns people have, and it’s often addressable with proper timing.
Timing guidance reduces next-day grogginess by aligning medication administration with your natural sleep window and morning commitments. A medication that works well for someone who sleeps from 10 PM to 6 AM might leave someone else foggy if they need to be sharp by 5 AM.
Timing Do’s and Don’ts:
Do:
- Allow a full sleep window (typically 7-8 hours) after taking your medication
- Take your medication at the same time each night to establish a rhythm
- Align timing with your actual schedule, not an ideal you’re trying to force
Don’t:
- Stack sedating behaviors right after your dose (like drinking alcohol or taking other sedating medications)
- Take your medication right before you need to wake up early
- Expect immediate perfection—timing often requires minor adjustments over the first few weeks
Your provider will help you find the right timing. If you notice grogginess, that’s valuable feedback. A simple schedule shift often solves the problem. For more detailed guidance, review our article on avoiding next-day grogginess with non-addictive sleep aids.
Eligibility and When Telehealth May Not Be Right
Certain situations require in-person evaluation for safety.
Online eligibility at SleepScript MD typically covers adults aged 18 to 65 without major medical, mental health, or substance use conditions that could make sleep medications unsafe. Pregnancy and plans to become pregnant are also exclusions because medication safety profiles change significantly during pregnancy.
Some sleep conditions need more comprehensive evaluation than telehealth can provide. Suspected narcolepsy requires specialized testing that includes overnight sleep studies. REM Sleep Behavior Disorder—where people physically act out their dreams—can be an early warning sign of neurological conditions and needs in-person neurological assessment. Complex Restless Legs Syndrome often has underlying causes like iron deficiency or kidney disease that require lab work and physical examination.
If you’ve been told you snore heavily, gasp for air, or stop breathing during sleep, you’ll need to complete an at-home sleep test before any treatment can begin. Medications are not prescribed until your test results are reviewed. This protects you from masking a more serious condition like obstructive sleep apnea.
For a complete list of conditions that require in-person care, visit our FAQ section on patients we can’t treat and review our eligibility criteria. All digital intake is HIPAA-compliant. To learn more about how federal privacy protections apply to telehealth, visit the U.S. Department of Health and Human Services HIPAA portal.
How to Get Started Today
Explore quick quizzes and educational resources before booking. You don’t need to commit to a full consult to start learning about your options.
Take the 2-Minute Sleep Clarity Quiz to clarify your goals and understand what type of sleep support might be most helpful. If you want to learn more about the specific safe sleeping pills used in telehealth sleep care — visit our treatments overview or explore our medication selection page. For answers to common questions about costs, insurance, and the consultation process, check our FAQ page.
When you’re ready to proceed, start your sleep treatment by beginning your intake. The entire process is HIPAA-compliant, and in most states where asynchronous care is permitted, you’ll often have clarity on next steps within the same day.
Frequently Asked Questions
What happens in a telehealth sleep consult?
A HIPAA-secure intake is reviewed by a licensed provider who screens for risks, tailors a medication plan, and—when appropriate—initiates or continues non-controlled prescription options. Follow-ups and refills are scheduled within a monthly subscription model to maintain continuity of care. The speed of this process may vary by state requirements.
How do refills and monthly subscriptions work?
Expect reminders, brief check-ins, and timely renewals to maintain continuity. The plan emphasizes ongoing clinician-managed care rather than short-term use—you stay on your medication as long as it’s helping, with monthly subscription support. For detailed pricing information, see our pricing page. Returning patients have a streamlined renewal process.
When is in-person care recommended?
If eligibility or safety screens flag concerns—such as pregnancy or breastfeeding, suspected narcolepsy, REM Sleep Behavior Disorder, complex Restless Legs Syndrome, or severe unstable medical or psychiatric conditions—providers direct care to in-person evaluation. See our FAQ section on patients we can’t treat for complete details.
Your Path to Reliable Sleep
Your consult sets you up for reliable sleep with ongoing, clinician-managed care—refills, monthly subscription support, and clear next steps. Safety-first means clinician review before prescription decisions, with a focus on non-controlled medications that help you sleep without dependency. Continuity of care means refills and a subscription model designed for long-term use, not a brief trial that stops after two weeks. Timing and follow-ups protect next-day clarity so you can show up sharp when it matters most.
You deserve sleep that works without the fear of dependency or the frustration of waking up foggy. That’s what a safety-first, medication-forward approach delivers.
Disclaimer: This article is informational and not a substitute for professional medical advice. Online care at SleepScript MD is available to eligible adults and may not be appropriate for all conditions. A licensed provider reviews each case before prescribing decisions are made.
Our Editorial Process
The SleepScript MD Insights Team synthesizes complex sleep topics into clear, helpful guides. Content is reviewed for clarity and accuracy and periodically updated to reflect our current safety standards and care model.
About the SleepScript MD Insights Team
The SleepScript MD Insights Team turns clinical guidance into practical, step-by-step resources so you can make informed decisions about safe, ongoing insomnia care.
