📌 Key Takeaways
Next-day grogginess isn’t inevitable—it’s usually the result of mistimed dosing that overlaps your waking hours.
The 8-Hour Rule Prevents Morning Fog: Plan roughly 8 hours between taking your sleep aid and your intended wake time to allow adequate clearance and avoid residual sedation.
Your Chronotype Determines Optimal Timing: Early birds and night owls can both use the same 8-hour window by aligning their dose with their natural bedtime, not an arbitrary clock time.
Stacking Sedatives Multiplies Grogginess Risk: Alcohol, antihistamines, and other sedating substances dramatically increase next-day impairment when combined with sleep aids.
Middle-of-the-Night Redosing Is a Trap: Taking another dose when fewer than 6-7 hours remain before wake time virtually guarantees morning grogginess and safety concerns.
Morning Light and Movement Accelerate Recovery: Bright light exposure, hydration, and brief movement within 30 minutes of waking help clear any remaining sleep inertia faster.
Strategic timing transforms sleep aids from a risky gamble into predictable rest without compromise.
The Science Behind Timing Sleep Aids Right
Residual sedation happens when a sleep aid’s effects overlap with your waking hours, creating that groggy, unfocused feeling the next morning. Picture trying to land an airplane—you begin your descent well before the runway so you touch down smoothly at exactly the right moment. The same principle applies to sleep medications.
You’re staring at the clock: 11:30 PM the night before your big presentation. You need rest, but you can’t afford to feel foggy during tomorrow’s meeting. This exact scenario drives many professionals to avoid sleep aids altogether, fearing they’ll wake up feeling worse than when they started.
The solution lies in understanding the “dose-to-wake window”—the time between taking a sleep aid and your planned wake time. When timed correctly, non-addictive sleep medications can provide the rest you need without compromising your next-day clarity.
The 8-Hour “Dose-to-Wake” Rule
Target approximately 8 hours between taking your sleep aid and your planned wake time. This window accounts for the typical time most adults spend in bed (7-9 hours) while allowing adequate clearance time for the medication to process through your system.
Consider Sarah, a marketing manager who needs to wake at 6:30 AM for an early client call. She takes her sleep aid at 10:30 PM, giving herself a full 8-hour window. By morning, the medication has had time to work through her system, and she wakes feeling refreshed rather than drowsy.
The key is consistency. If your bedtime shifts, move your dose timing accordingly to maintain that 8-hour buffer.
Adjusting for Your Natural Sleep Pattern
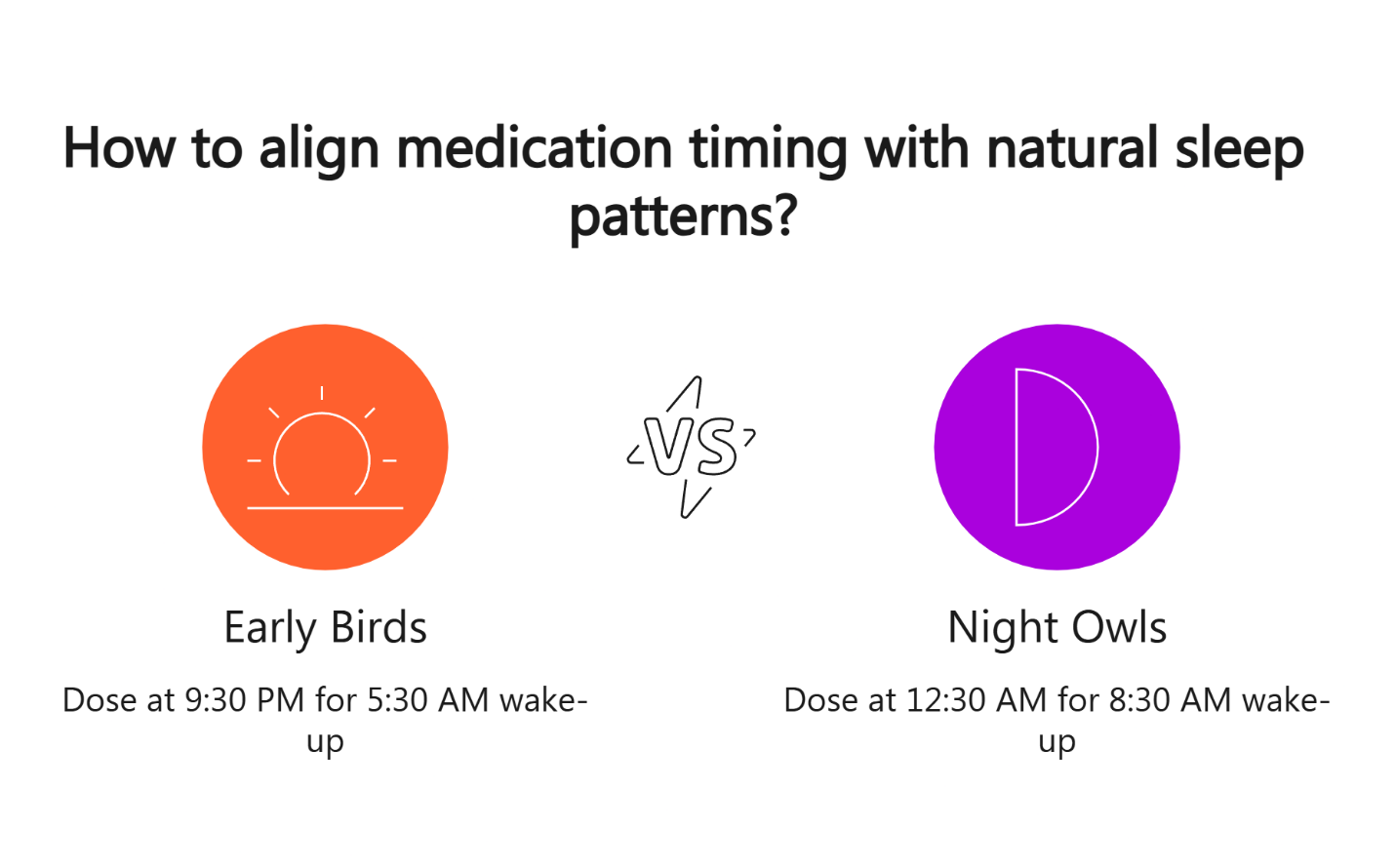
Keep the same 8-hour window but align your dose with your natural bedtime preferences. Your chronotype—whether you’re naturally an early bird or night owl—affects when you feel most alert or sleepy, but the timing principle remains constant.
Early risers might dose at 9:30 PM for a 5:30 AM wake time, while natural night owls could take their medication at 12:30 AM for an 8:30 AM alarm. Both maintain the protective 8-hour window while respecting their body’s natural rhythm.
Consistency matters more than the specific clock time. Find your optimal schedule and stick with it, even on weekends when possible.
Pre-Dose Timing Checklist
Before taking your sleep aid tonight:
- Block an 8-hour sleep window from dose to wake time
- Finish dinner 2-3 hours before dosing (light snack okay if needed)
- Avoid alcohol within several hours of your planned dose
- Complete screen time and mentally demanding tasks before dosing
- Set your morning alarm and plan for natural light exposure
What Not to Combine with Your Sleep Aid
Avoid stacking sedating substances near your dose time. Combining sleep aids with alcohol, antihistamines, or other sedatives significantly increases your risk of next-day grogginess and can create dangerous interactions.
If you’ve had alcohol with dinner, skip your sleep aid that night and resume your routine when alcohol-free. The interaction between alcohol and sleep medications can extend sedation well into the next day, affecting your coordination and decision-making abilities.
Heavy meals within 2-3 hours of dosing can also affect how your body processes the medication, potentially extending its effects into morning hours.
What to Avoid Near Dose Time
- No combining with other sedatives or antihistamines unless directed by your clinician
- Skip late caffeine “rescues” that might delay natural sleep onset
- Avoid new supplements on nights you’re testing timing
Why Middle-of-the-Night Redosing Is Risky
If you wake at 2 or 3 AM and fewer than 6-7 hours remain before your alarm, resist the urge to take another dose. Redosing with insufficient clearance time almost guarantees morning grogginess and can impair your ability to drive safely or make important decisions.
Instead of redosing, try gentle breathing exercises, avoid checking the time repeatedly, and use basic sleep hygiene techniques to encourage natural return to sleep. Many people find that accepting occasional middle-of-the-night wakefulness without anxiety helps them drift back off naturally.
Always consult your clinician about safe redosing protocols if middle-of-the-night waking becomes a pattern.
Your First Three Nights Strategy
Start testing your timing on low-stakes nights when next-day performance isn’t critical. This allows you to observe how the medication affects you personally without risking important obligations.
Keep your timing consistent across these test nights. Take your sleep aid at the same time, aim for the same bedtime, and wake at your usual hour. Track your morning alertness on a simple 0-10 scale where 0 is completely groggy and 10 is fully alert.
Example Three-Night Log:
- Night 1: Dose 10:30 PM, sleep 11:00 PM, wake 6:30 AM, morning alertness: 7/10
- Night 2: Dose 10:30 PM, sleep 10:45 PM, wake 6:30 AM, morning alertness: 8/10
- Night 3: Dose 10:30 PM, sleep 11:15 PM, wake 6:30 AM, morning alertness: 6/10
Bring this information to your follow-up consultation. Your clinician can help adjust timing or dosage based on your real-world response patterns.
Morning Reset Routine to Clear Sleep Inertia
Even with perfect timing, most people experience some degree of sleep inertia—that natural grogginess immediately upon waking. A simple morning routine can help accelerate the transition to full alertness.
Get bright light exposure within 30 minutes of waking. Open blinds, step outside briefly, or use a light therapy device. Light signals your brain to suppress any remaining melatonin and shift into daytime alertness mode.
Follow light exposure with hydration and gentle movement. Even 2-5 minutes of light stretching or walking helps circulate the medication out of your system and increases blood flow to your brain.
Morning Reset Steps
- Get bright light within 30 minutes of waking
- Hydrate immediately upon getting up
- Do 2-5 minutes of gentle movement or stretching
- Delay driving or important decisions until you feel fully alert
Safety Guidelines and When to Check In
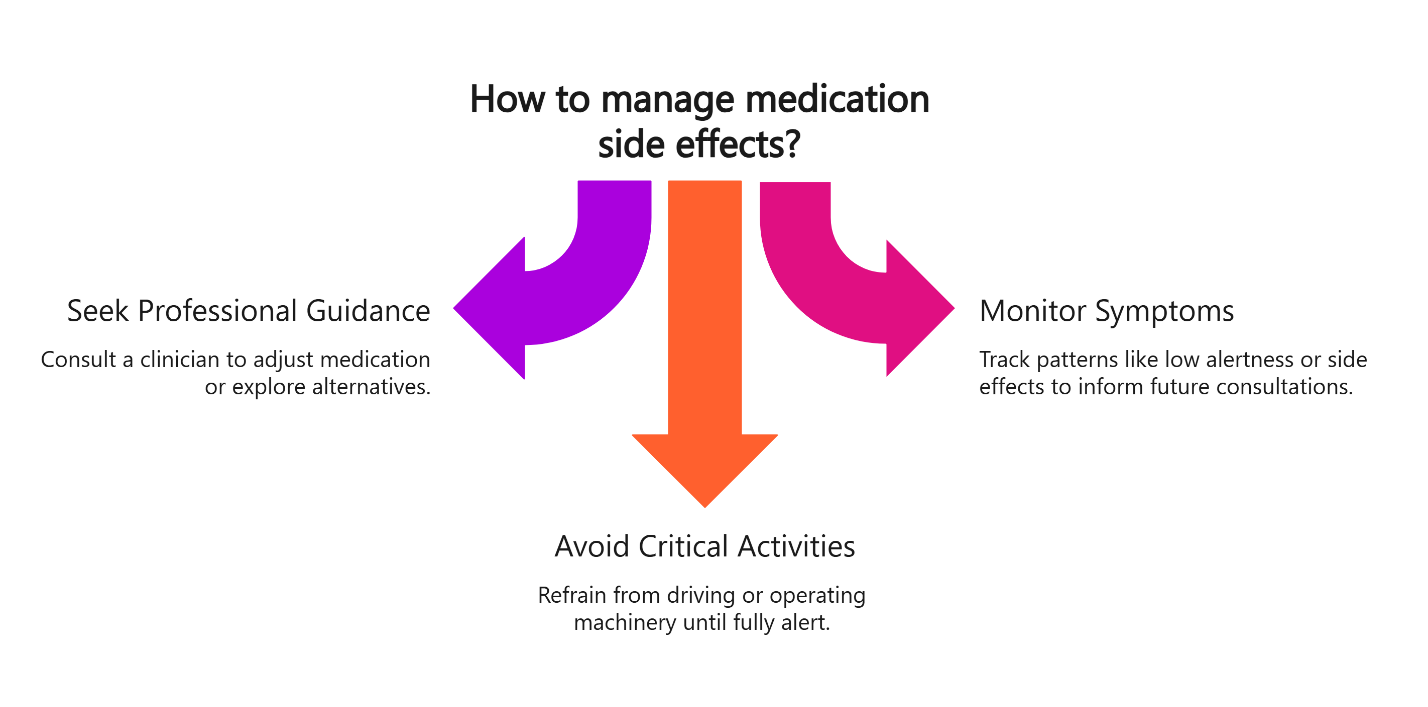
Don’t attempt to self-adjust your medication if you experience persistent morning grogginess, dizziness, or any symptoms that could affect safety-critical activities like driving. These signs indicate you need professional guidance to optimize your treatment.
Schedule a follow-up consultation if you notice patterns like consistently low morning alertness scores, difficulty staying asleep despite the medication, or any concerning side effects. Your clinician can adjust dosing, timing, or explore alternative medications that might work better with your body chemistry.
Never drive, operate machinery, or make important decisions until you feel completely alert. The responsibility for recognizing your level of impairment lies with you, regardless of how long it’s been since your dose.
When to Contact Your Clinician
- Persistent grogginess lasting more than 2-3 hours after waking
- Dizziness or coordination problems the next day
- No improvement in sleep quality after consistent use
- Any safety concerns about next-day alertness
Taking Control of Your Sleep Without Compromise
The fear of next-day fogginess keeps many people trapped in cycles of poor sleep and declining performance. With proper timing and guidance, non-addictive sleep aids can provide the rest you need while preserving your morning clarity and professional effectiveness.
Remember that this process requires patience and fine-tuning. What works perfectly for your colleague might need adjustment for your body and schedule. The key is systematic tracking, open communication with your clinician, and commitment to the safety protocols that protect both your sleep and your waking life.
Your sleep shouldn’t come at the cost of tomorrow’s performance. Start with low-stakes nights, follow the 8-hour rule, and build the confidence that comes from knowing you can rest well and wake ready.
Timing Do’s and Don’ts Quick Reference
DO:
- Aim for roughly 8 hours between dose and wake time (most adults target 7-9 hours in bed)
- Keep lights-out consistent and shift dose if bedtime shifts
- Test on low-stakes nights; bring 3-night logs to your follow-up
- Use a morning reset: bright light, hydration, brief movement
DON’T:
- Redose after midnight (or when fewer than 6-7 hours remain) without clinician guidance
- Combine with alcohol or other sedatives
- Drive or make heavy decisions until fully alert
Seasonality Watch
Daylight Saving Time shifts (March and November), back-to-school transitions (August–September), and holiday season changes (November–December) can disrupt bedtimes. Protect the interval: if wake time changes by an hour, adjust dose time by the same hour for the next few nights.
Frequently Asked Questions
How many hours before waking should a sleep aid be taken?
Most adults benefit from about 8 hours between dose and planned wake time; clinicians may tailor this based on response.
Can another dose be taken at 2–3 a.m.?
Generally no if fewer than 6-7 hours remain. Ask your clinician for case-specific guidance.
What if alcohol was consumed?
Skip the dose and resume on a night without alcohol; mixing raises grogginess and safety risks, consistent with CDC sleep guidance.
Do timing rules change by chronotype?
Keep the same 7-9 hour window; align dose with your natural bedtime. Fine-tune during follow-ups.
How should timing and morning alertness be logged?
Track dose time, time in bed, wake time, and 0-10 alertness. Share logs during telehealth check-ins to refine timing.
Our Editorial Process
All SleepScriptMD content is created for clarity and usefulness, then reviewed for accuracy and alignment with our safety-first prescribing policies. When we cite research or clinical guidelines, we prioritize reputable, non-commercial sources. Articles are periodically updated for relevance and readability.
About the SleepScriptMD Insights Team
The SleepScriptMD Insights Team synthesizes complex sleep topics into clear, helpful guides. While reviewed for clarity and accuracy, this content is informational and not a substitute for professional medical advice.
This guide is informational and not medical advice. It does not replace a clinician’s judgment or your own provider’s instructions. Do not drive or operate machinery unless fully alert. If you experience concerning symptoms, contact a healthcare professional.
