📌 Key Takeaways
Persistent insomnia affecting work performance benefits from supervised, non-controlled prescription care when OTC trial-and-error creates more problems than it solves.
- Frequency Plus Impact Signals Escalation: If sleep trouble occurs three or more nights weekly and affects next-day function, supervised care often outperforms continued OTC experimentation.
- Timing Windows Protect Mornings: Clinicians select medications with clearance rates matching your wake schedule, then calculate precise dosing times—not just better instructions, but better-matched pharmacology.
- Pattern-Fit Eliminates Guessing: Identifying whether you struggle with sleep onset or sleep maintenance determines which non-controlled medication targets your specific insomnia mechanism.
- Safety Screening Catches Hidden Issues: Physician review identifies conditions like sleep apnea or narcolepsy that require testing rather than medication, protecting you from masking treatable problems.
- Gradual Adjustment May Be Needed: While non-controlled options don’t carry high abuse risk, some medications may require tapering rather than abrupt stopping to avoid rebound effects.
Prepared screening + matched medication = predictable nights without next-day fog.
Adults managing persistent insomnia who want to stop shuffling through OTC products will gain clarity on when supervised care makes sense, preparing them for the detailed process overview that follows.
You’ve optimized everything: blackout curtains, white noise, no screens after 9 PM. Still, here you are at 2 AM, calculating how many hours you might get if you fall asleep right now. The melatonin and magnesium bottles sit on your nightstand—reminders of another night spent guessing.
Here’s what makes the difference: supervised, non-controlled prescription sleep care works like installing the right autopilot for your nights. Instead of tweaking settings on your own through trial-and-error, you get predictable sleep and clear mornings through timing windows and safety-first guidance—eliminating the cycle that leaves you foggy when it matters most.
This isn’t about choosing between “natural” and “chemical.” It’s about recognizing when persistent insomnia calls for a reliable, evidence-based solution rather than shuffling through OTC options and hoping one finally works.
The Quick Answer: OTC Can Be Fine Short-Term—Persistent Insomnia Usually Needs a Supervised Plan
If you’ve been using over-the-counter sleep aids for more than a few weeks with inconsistent results, you’re experiencing what most people do: OTC remedies work well for occasional sleeplessness but weren’t designed for the kind of persistent insomnia that affects your next-day performance.
The distinction isn’t about severity—it’s about pattern. Situational insomnia (jet lag, a stressful event, a schedule disruption) responds well to short-term OTC support. Persistent insomnia (three or more nights per week for several weeks) typically benefits from a pattern-fit solution that accounts for whether you struggle to fall asleep, stay asleep, or both.
A Simple Rule of Thumb: Frequency + Next-Day Impact
Ask yourself two questions:
- How often? If you’re reaching for sleep support more than three nights per week, the pattern suggests your body needs more than an occasional nudge.
- How’s tomorrow? If you’re waking up groggy, struggling through morning meetings, or organizing your entire day around compensating for rough sleep, you’ve crossed into territory where guesswork becomes costly.
When both answers point to “regular” and “affecting my performance,” it’s time to stop experimenting and start working with a clinician who can match your specific pattern to a safe, effective solution.
When Supervised Care Makes Sense: Decision Tree
Start here: Are you struggling to sleep 3 or more nights per week?
- No → OTC or sleep hygiene adjustments may still work. Consider trying a consistent routine for 2-3 weeks.
- Yes → Continue below.
Has this pattern lasted more than a few weeks despite good sleep habits?
- No → You may be experiencing situational insomnia. OTC support + addressing the stressor may be sufficient.
- Yes → Continue below.
Does morning grogginess or next-day fatigue affect your work or daily life?
- No → Your current approach may be working well enough. Monitor for changes.
- Yes → Continue below.
Have you tried multiple OTC options without consistent results?
- No → Consider one more targeted OTC trial with attention to timing and interactions.
- Yes → You’re a candidate for supervised, non-controlled prescription care.
Next steps:
- Take the 6-Second Sleep Check for a quick assessment.
- Start Your Sleep Treatment to begin a clinician-guided plan.
OTC Sleep Remedies: What They Help, Where They Fall Short
Over-the-counter sleep aids fall into three broad categories: antihistamine-based options (like diphenhydramine), melatonin supplements, and herbal blends (valerian, chamomile, magnesium combinations). Each works through a different mechanism, which explains why someone’s enthusiastic recommendation might do nothing for you.
Common OTC Categories
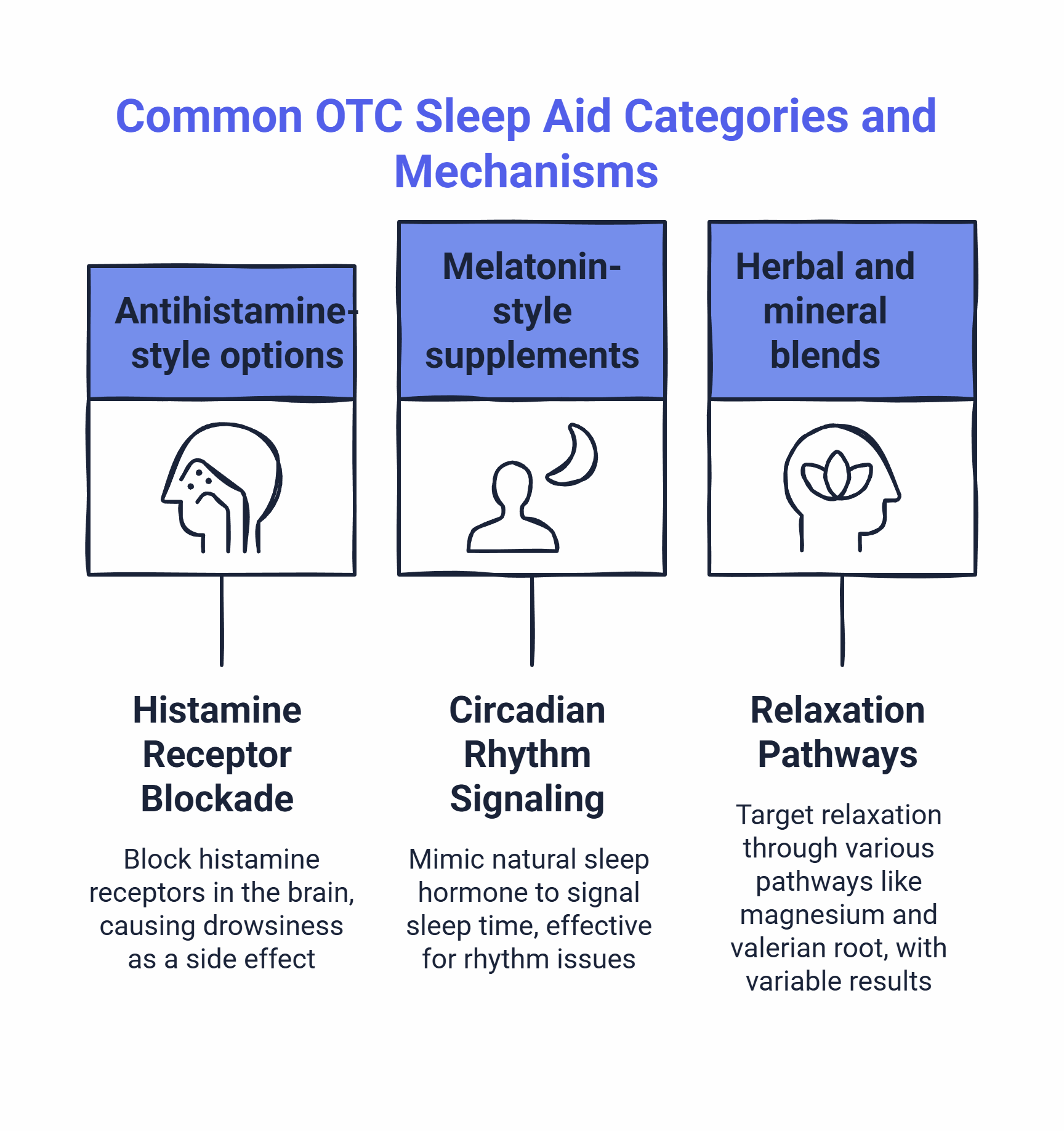
Antihistamine-style options work by blocking histamine receptors in your brain, creating drowsiness as a side effect. They’re predictable for occasional use but build tolerance quickly—what worked last week might feel like nothing this week.
Melatonin-style supplements signal to your body that it’s time to sleep by mimicking your natural sleep hormone. They work well for circadian rhythm issues (shift work, travel) but don’t force sleep the way sedatives do. If your mind is racing, melatonin alone often isn’t enough.
Herbal and mineral blends (magnesium, valerian root, L-theanine) target relaxation through various pathways. Quality and absorption vary widely between brands, making results unpredictable even when you’re taking the “right” ingredients.
Why OTC Often Turns Into Trial-and-Error
The core problem: these options weren’t designed with your specific insomnia pattern in mind. You’re essentially running your own informal clinical trial every night, adjusting doses, trying combinations, and hoping the next stack works better than the last.
This creates decision fatigue at the worst possible time—when you’re already exhausted and need to function tomorrow. You start second-guessing: “Did I take it too late? Should I have doubled the magnesium? Was it the blue light from checking my phone at 10:30?”
Without supervision, it’s easy to chase a different product each week without answering the underlying pattern question: Is the issue sleep onset (falling asleep)? Sleep maintenance (staying asleep)? Timing (sleeping at the wrong times for your wake schedule)? Or something else that should be screened first (like breathing disruptions)?
Common Reasons OTC Leads to Morning Fog or ‘Half-Sleep’
Morning grogginess with OTC remedies usually comes from one of three issues:
- Timing mismatch: You took it too late, and the active window extends into your wake time.
- Dose uncertainty: Without guidance, you’re guessing at the amount, often taking more than needed.
- Interaction effects: Combining multiple OTC products or mixing them with alcohol or late caffeine compounds the sedative effect.
The frustration isn’t that these products don’t work—it’s that they work unpredictably, leaving you managing variables you didn’t know existed.
OTC vs. Supervised Non-Controlled Prescription Care—Comparison
Factor | OTC Remedies | Supervised Non-Controlled Prescription |
|---|---|---|
Best for | Occasional, situational sleeplessness (travel, stress events) | Persistent insomnia (3+ nights/week for several weeks) |
Speed of effect | Varies; melatonin signals sleep onset, antihistamines sedate within 30-60 min | Typically works within 30-60 min; pattern-fit to onset vs. maintenance needs |
Predictability | Inconsistent; tolerance builds with antihistamines | Consistent when paired with timing windows and what-to-avoid rules |
Common morning-fog drivers | Late dosing, dose uncertainty, product stacking | Eliminated through clinician-set timing windows and avoid-list guidance |
Safety screening | Self-assessed; interactions often missed | Physician-reviewed; screens for sleep apnea, contraindications, interaction risks |
When it makes sense | Brief, situational sleep trouble | Frequent insomnia affecting next-day performance |
When Supervised, Non-Controlled Prescription Options Make Sense
Supervised prescription care isn’t about escalating to something “stronger”—it’s about choosing a reliable, evidence-based approach from the start. When medication is necessary, non-controlled options like trazodone, hydroxyzine, and clonidine are frequently prescribed off-label as initial pharmacological treatments for persistent insomnia, often when Cognitive Behavioral Therapy for Insomnia (CBT-I) isn’t accessible or sufficient. The decision point arrives when the energy you’re spending on managing your sleep is affecting the life you’re trying to protect.

If You’ve Tried Basic Sleep Hygiene and Still Can’t Fall or Stay Asleep
You’ve already done the work: consistent sleep schedule, dark room, cool temperature, no caffeine after 2 PM. These habits create the conditions for sleep, but they don’t force it. When your body or mind won’t cooperate despite good conditions, the problem isn’t your effort—it’s that your specific insomnia pattern benefits from a targeted solution.
A clinician-guided approach starts by identifying whether you struggle with sleep onset (falling asleep) or sleep maintenance (staying asleep). This distinction matters because different medications work through different mechanisms. You stop guessing and start using a solution designed for your pattern.
If Grogginess Is the Main Fear (Timing Windows Matter More Than You Think)
The number one concern people have about prescription sleep support: “Will I feel drugged tomorrow?” This fear keeps many people stuck in the OTC trial-and-error loop far longer than necessary.
Here’s what changes the equation: supervised care includes explicit timing windows that protect your mornings. Your clinician calculates when to take your medication based on your wake time, not a generic “take at bedtime” instruction. This precision—combined with knowing what to avoid (alcohol, late caffeine, blue-light devices before bed)—is what prevents the grogginess you’re trying to avoid.
The difference between waking up groggy and waking up clear often comes down to 30 to 45 minutes of timing adjustment and a short list of behavioral guardrails.
If Anxiety, Travel, or Unpredictable Schedules Keep Breaking Your Routine
For people whose sleep is disrupted by variable schedules—shift workers, frequent travelers, or anyone whose stress levels swing unpredictably—OTC remedies become another thing to manage rather than a reliable solution.
Supervised, non-controlled prescription options provide a consistent baseline. You’re not recalculating doses based on stress levels or travel fatigue. You have a clear protocol: take it within your timing window, follow your avoid list, and track your morning clarity. When your schedule changes (time zone shifts, daylight saving time), your clinician adjusts the plan rather than leaving you to experiment.
What Supervised Care Actually Looks Like (and Why It’s Safer Than Guessing)
The process is designed to eliminate the variables that make OTC approaches frustrating. You’re not navigating this alone, and you’re not skipping steps that protect your safety.
Safety Screening: Who Should Seek In-Person Evaluation First
Before any prescription is considered, you’ll complete a screening that identifies conditions requiring more specialized care. This ensures you’re getting the right type of support for your specific situation.
You’ll need in-person evaluation if you experience:
- Loud snoring, gasping, or breathing pauses during sleep (potential sleep apnea—requires testing)
- Sudden daytime sleep attacks or muscle weakness during strong emotions (possible narcolepsy)
- Acting out dreams physically during sleep (REM sleep behavior disorder)
- Uncomfortable leg sensations that prevent sleep (restless legs syndrome)
If any of these apply, the screening routes you to appropriate testing or specialist care. This protects you from treating symptoms without addressing the underlying condition.
Important: SleepScriptMD treats low-risk adults ages 18-65. We do not treat individuals who are pregnant, planning pregnancy, or have certain medical conditions that require in-person monitoring. The screening process clarifies eligibility upfront.
Pattern-Fit Approach: Onset vs. Maintenance
Once safety screening is complete, your clinician identifies your primary pattern:
Sleep onset difficulty (trouble falling asleep) typically responds to medications that work quickly and clear your system by morning. The goal is to help you fall asleep within 30 to 60 minutes without extending sedation into your wake time.
Sleep maintenance difficulty (waking frequently or too early) typically benefits from medications that support deeper, continuous sleep throughout the night. These are selected for their ability to extend your natural sleep architecture without creating morning grogginess.
Many people have both patterns. Your clinician prioritizes the pattern causing the most next-day impact and adjusts from there.
The ‘First 7 Nights’ Expectation-Setter
Supervised prescription sleep care often shows improvement within the first few nights, but the first week is about calibration, not perfection. You’re establishing your baseline and identifying any adjustments needed.
What to expect during the first 7 nights:
- Nights 1-3: Notice whether you’re falling asleep more predictably. Track your morning clarity (we’ll cover this below).
- Nights 4-7: Your body adjusts to the new pattern. Small timing or behavioral adjustments may improve results.
- After night 7: You should have a clear sense of whether the approach is working or if adjustments are needed.
This isn’t a promise of instant perfection—it’s a structured observation period that tells you and your clinician what’s working.
How to Protect Your Mornings: The 3 Levers
Morning clarity isn’t luck—it’s the result of three controllable factors that most people manage unconsciously with OTC remedies and precisely with supervised care.
Lever 1: Timing Window
Your medication has a predictable active window (the time it takes to work and clear your system). Your clinician selects a medication with a duration of action that matches your sleep opportunity, then calculates when you should take it based on your typical wake time. This ensures the medication clears your system before your alarm rings.
Example: If you need to be clear-headed by 6:30 AM, your timing window might be 10:00 to 10:30 PM. Taking it at 11:30 PM pushes the tail end of the active window into your wake time, creating the grogginess you’re trying to avoid.
This is different from OTC approaches, where you can time a pill perfectly but still wake up groggy if it has a long half-life. With supervised care, the medication itself is chosen to match your schedule—not just the timing of when you take it.
Travel and daylight saving adjustments: Your timing window shifts with your schedule. If you travel across time zones or adjust for daylight saving time, your clinician helps you recalculate rather than leaving you to guess.
Lever 2: What to Avoid (The Morning-Protection Checklist)
Certain substances and behaviors compound the sedative effect of sleep medication or disrupt your natural sleep architecture, leading to that groggy, “half-asleep” feeling in the morning.
The short avoid list:
- Alcohol within 4 hours of your dose: Alcohol amplifies sedation and disrupts REM sleep, creating fragmented rest even if you “sleep” longer.
- Caffeine after 2 PM: Even if you don’t feel wired, late caffeine prevents the deep sleep stages where your body and brain restore.
- Blue-light devices after your dose: Screens signal wakefulness to your brain, working against the medication’s effect and delaying sleep onset.
These aren’t lifestyle restrictions—they’re temporary guardrails during your active treatment window. You’re protecting the investment you’re making in your sleep.
Lever 3: Morning Clarity Score (1-10) + Adjustment Loop with Clinician Guidance
This is the feedback mechanism that makes supervised care iterative rather than static. Each morning, you briefly assess your clarity on a simple 1-10 scale:
- 1-3: Groggy, difficult to function, needed extra time to feel clear
- 4-6: Somewhat foggy, manageable but not ideal
- 7-10: Clear-headed, energized, ready for your day
The adjustment loop (3 steps):
Step | Action | Notes |
|---|---|---|
1. Track | Rate your morning clarity (1-10) for 5-7 days | Patterns emerge; one rough morning isn’t a signal to change everything |
2. Identify patterns | If you’re consistently below 7, identify the variable (timing? avoid-list slip? dose?) | Most issues resolve with timing or behavior adjustments, not dose changes |
3. Adjust with clinician | Report your pattern; your clinician guides timing or behavior changes first, dose adjustments only if needed | Small changes create big results when they’re the right changes |
This isn’t trial-and-error—it’s structured observation with expert guidance. You stop guessing and start adjusting based on data.
Cost and Convenience: Online Intake, State Variation, and Practical Next Steps
Supervised care through platforms like SleepScriptMD is designed to remove the friction that keeps people stuck in OTC loops. The process is straightforward, and the costs are transparent.
Asynchronous Online Care vs. Virtual Visits
Asynchronous care (available in most states): You complete a detailed online intake at your convenience. A licensed clinician reviews your information, and if you’re eligible, a prescription is often sent to your pharmacy the same day. This works well for straightforward insomnia patterns without complex medical histories.
Virtual visits (required in some states or for complex cases): You schedule a video consultation with a clinician. This is recommended if you have multiple medical conditions, take several medications, or have tried sleep medications before without success. The visit provides more back-and-forth discussion and personalized guidance.
Both pathways include safety screening and clinician oversight. The difference is timing and interaction style, not quality of care. State telehealth regulations vary, so the intake process will clarify your state’s requirements upfront.
Prescription Sent to Your Pharmacy (Cost Separate)
Your clinician sends your prescription electronically to the pharmacy you choose. You pay for the medication separately when you pick it up—this cost is not included in your care fee and varies based on your insurance coverage and the specific medication prescribed.
Most non-controlled sleep medications like trazodone, hydroxyzine, and clonidine are generic and widely covered by insurance, making them more affordable than many people expect. If cost is a concern, your clinician can discuss options and help you find the most cost-effective solution.
For detailed pricing information about the care platform itself, visit the pricing page.
State Variation Note
Telehealth rules differ by state. Some states allow fully asynchronous care for non-controlled sleep medications; others require at least one video visit before prescribing. The intake process will clarify your state’s requirements upfront—no surprises, no hidden steps.
FAQs (Fast Answers, No Scare Tactics)
Will I feel drugged tomorrow?
Not if the timing window and avoid list are followed. Morning grogginess happens when medication is taken too late (pushing the active window into your wake time) or when it’s combined with alcohol or other sedatives. Your clinician sets your timing window specifically to clear your system before you need to be alert. Most people report feeling more rested—not groggy—because they’re finally getting continuous sleep.
Is it habit-forming?
Non-controlled prescription sleep medications (the type prescribed through supervised care platforms) do not carry the high risk of abuse or addiction associated with controlled substances. While they are not classified as habit-forming, some medications may require a gradual taper rather than abrupt stopping to avoid rebound effects. The goal is to use them as a bridge while you establish better sleep patterns, not as a permanent solution.
What if I have snoring or breathing issues at night?
If you snore loudly, gasp for air, or have been told you stop breathing during sleep, you may have sleep apnea—a condition that requires testing, not sleep medication. The screening process will identify this risk and route you to appropriate testing (often a simple at-home sleep study). This ensures you’re treating the right condition.
How soon should I expect results?
Most people notice improved sleep within the first 2-3 nights. By the end of the first week, you should have a clear sense of whether the approach is working. If you’re not seeing improvement by night 7, your clinician adjusts the plan—this is normal and expected. The goal is consistent results, not a one-size-fits-all prescription.
Can I travel with my medication?
Yes. Non-controlled medications don’t have the travel restrictions that controlled substances do. Keep your medication in its original pharmacy bottle with your name on the label. If you’re crossing time zones, adjust your timing window to align with your new wake time—your clinician can help you calculate this.
What if I miss a dose?
If you miss a night, simply resume your regular schedule the next night. Don’t double up or take it late to “catch up.” Your sleep pattern may be slightly disrupted for one night, but this won’t undo your progress. Consistency matters more than perfection.
What are common side effects?
Common side effects vary by medication but may include mild drowsiness, dry mouth, or slight morning grogginess that improves with timing adjustments. Your clinician will review what to expect with your specific medication. If you experience any concerning symptoms, contact your provider for guidance.
What if the medication stops working after a while?
If you notice your medication becoming less effective, contact your clinician before making changes. This could signal a change in your underlying sleep pattern or new stressors affecting your sleep. Your clinician adjusts the approach based on what’s driving the change—sometimes a small timing shift is all that’s needed.
Which Medication Is Right for Your Sleep Pattern?
SleepScriptMD offers three non-controlled prescription sleep aids selected for their effectiveness and favorable safety profiles:
Trazodone — Often used for middle-of-night waking and sleep maintenance. It is thought to support sleep architecture; clinical observations suggest many patients notice sedative effects immediately, though finding the optimal dosage may take time.
Hydroxyzine (Vistaril) — Best for anxiety-related insomnia and racing thoughts. Calms overactive nervous system; works in 15-30 minutes.
Clonidine — Best for stress-related sleep issues and ADHD-related insomnia (Off-label). Originally an antihypertensive, it reduces stress hormones and helps you transition to sleep in 30-60 minutes.
Your clinician will help you choose the right medication based on your specific sleep pattern during your intake. You can also explore detailed information about each medication on our Medication Selection Page.
Next Steps: Install Your Night-Time Auto-Pilot (Without Guesswork)
You’ve spent enough nights calculating sleep hours and organizing your day around fatigue. The decision isn’t whether you deserve help—it’s whether you’re ready to stop managing variables you can’t control and start working with a solution that’s designed to work.
Non-controlled prescription sleep care eliminates the trial-and-error cycle that keeps you awake worrying about tomorrow. You get a pattern-fit solution, explicit timing windows, and a clear avoid list. Most importantly, you get a clinician who adjusts the plan with you rather than leaving you to guess.
Ready to start treatment?
- Start Your Sleep Treatment — Complete a confidential intake and get clinician review (often same-day prescription in most states)
- See Which Medications We Offer — Learn about trazodone, hydroxyzine, and clonidine
- Quick Fit Check — See if you qualify (takes 2 minutes)
- View Pricing — Transparent costs with no hidden fees
Want to assess your sleep pattern first?
Start with a quick quiz to understand what’s affecting your rest:
- Take the 6-Second Sleep Check — A fast gut-check on whether your sleep pattern warrants next steps
- Try the Sleep Clarity Quiz — A more detailed assessment of what’s disrupting your sleep
- The Deep Sleep Profiler — Comprehensive screening for multiple sleep issues
The nights you’ve spent awake aren’t a reflection of your effort. They’re a signal that your specific insomnia pattern would benefit from a reliable, evidence-based approach rather than shuffling through OTC options and hoping one finally works. That approach exists, and it starts with one conversation with a clinician who understands the difference between occasional sleeplessness and persistent insomnia.
Your next clear morning is closer than you think.
Disclaimer
This article is for educational purposes only and is not medical advice. Prescription decisions, side effects, and interactions are individual—talk with a licensed clinician for personal guidance. If you’re experiencing severe symptoms, contact your healthcare provider.
Our Editorial Process
Our content is created by the SleepScriptMD Insights Team using a safety-first editorial workflow. We start with the clinical question readers are actually asking, review reputable medical references, and align guidance with how clinician-supervised sleep care works in practice. Articles are written for clarity (not jargon), prioritize practical next steps (like timing windows and what-to-avoid checklists), and are reviewed for accuracy, tone, and compliance before publishing. Content is educational and may be updated as standards of care and telehealth rules evolve.
By: The SleepScriptMD Insights Team
The SleepScriptMD Insights Team synthesizes complex sleep medicine topics into clear, helpful guides. Content is educational and not a substitute for medical advice.
