📌 Key Takeaways
Morning grogginess from prescription sleep aids usually signals a timing problem, not a medication problem.
- Consistency Beats Strength: Taking your medication within the same 30-minute window each night prevents unpredictable wake-up clarity more reliably than dosage changes.
- Track With a 1-10 Score: Rating your morning alertness daily for seven nights reveals the timing pattern that works for your body.
- Small Shifts Solve Big Problems: Moving your dose just 15-30 minutes earlier typically eliminates grogginess without switching medications.
- Anchor to One Nightly Cue: Linking your dose to a fixed action—like brushing teeth or docking your phone—removes decision fatigue and stabilizes your sleep schedule.
- Avoid Alcohol Four Hours Before: Skipping alcohol near bedtime protects both medication effectiveness and morning clarity.
Timing first, adjustments second, switches last.
Adults taking non-addictive prescription sleep medications who want sharper mornings will find practical calibration steps here, preparing them for the detailed timing protocols that follow.
What Timing Windows Actually Mean for Your Morning
Picture this: tomorrow holds a presentation you cannot afford to stumble through. You took the step to get a safe sleeping pill prescribed by your doctor. The medication sits on your nightstand, ready to help. Now you just need to know: when exactly should you take it to wake up sharp instead of foggy?
A timing window is the specific 30–60 minute period before your target bedtime when you take your prescribed sleep medication. Think of it like setting a nighttime routine. The medication needs enough time to work with your natural sleep drive, helping you fall asleep smoothly and wake up refreshed.
The good news: getting this right is simpler than most people expect. The difference between a clear morning and a groggy one often comes down to a 15–30 minute shift in when you take that tablet. You can lock in a simple routine during your first week, track your results with a quick morning score, and adjust based on what your body tells you.
Important: This content is educational and does not constitute medical advice. Always follow your clinician’s specific guidance regarding medication timing and dosage.
“Consistency beats dosage changes—most grogginess is a timing issue.”
Why These Medications Work (and Why Timing Matters)
The non-addictive sleep medications prescribed by SleepScriptMD—including trazodone, hydroxyzine, and clonidine—are proven, effective options that help you fall asleep and stay asleep without the risk of dependency. These aren’t controlled substances. They’re safe, evidence-based medications used by millions of people to restore healthy sleep patterns.
The key to getting the most from your prescription sleep aid is taking it at a consistent time each night. When you do this, your body learns to anticipate sleep at the right moment, and the medication clears your system by morning—leaving you alert and ready for the day.
Bedtime-Anchored Dosing vs. Ad-Hoc Timing
Taking your medication at random times based on when you feel tired creates unpredictable results. Your body cannot establish a rhythm when the signal keeps moving.
Bedtime-anchored dosing ties your dose to a single, repeatable cue each night. This might be right after brushing your teeth or immediately after docking your phone on the charger across the room. The cue stays constant. The medication enters your system at the same point in your wind-down every single night.
This consistency allows your body to anticipate sleep. The medication works with your circadian rhythm rather than fighting against whatever random hour you decided to try sleeping.
The 1–10 Morning Clarity Score Loop
For your first seven nights, rate your morning clarity on a simple 1–10 scale the moment you wake up. A 10 means you feel completely alert and ready. A 1 means you can barely function.
This score becomes your feedback mechanism. Most adults starting non-controlled sleep medications find their sweet spot within the first week by paying attention to this number and making small adjustments.
Write down three things each morning: what time you took your dose, what time you actually fell asleep, and your clarity score. Patterns emerge quickly.
The “Clock Problem” Myth
Many people assume grogginess means the medication is too strong or simply wrong for them. They want to switch drugs or abandon the approach entirely.
Here is what actually happens in most cases: the timing is off by 30–45 minutes. The medication’s effects peak either too early (leaving you alert at 2 AM) or too late (leaving residual sedation at 7 AM). A timing adjustment often resolves what feels like a medication problem.
Before concluding that a prescription sleep aid does not work, spend a full week fine-tuning your timing window. The results frequently surprise people who were ready to give up.
The Timing Window Cheat Sheet
This table provides general starting points and is designed to be screenshot-friendly for easy reference. Your clinician may recommend different windows based on your specific situation and the medication prescribed. Learn more about which medication might be right for you.
Target Bedtime | Early Window | Standard Window | Late Window | Expected AM Feel | If Clarity <7 |
|---|---|---|---|---|---|
10:00 PM | 8:30–9:00 PM | 9:00–9:30 PM | 9:30–10:00 PM | Alert by 6 AM | Move 15–30 min earlier |
11:00 PM | 9:30–10:00 PM | 10:00–10:30 PM | 10:30–11:00 PM | Alert by 7 AM | Move 15–30 min earlier |
12:00 AM | 10:30–11:00 PM | 11:00–11:30 PM | 11:30 PM–12:00 AM | Alert by 8 AM | Move 15–30 min earlier |
Accessibility note: Timing window reference table showing dosing windows relative to target bedtime for minimizing next-day grogginess
How to use this table: Start with the standard window for your target bedtime. After rating your morning clarity, adjust in 15–30 minute increments until you consistently score 7 or higher.
The 4-Step Adjustment Loop
- Rate your clarity on waking (1–10 scale)
- If your score falls below 7, move your dose 15–30 minutes earlier tonight
- If you score 8+ but experience early-morning awakenings (waking at 4 AM unable to return to sleep), move your dose 15–30 minutes later
- Repeat this process nightly for seven nights. Contact your clinician if you experience anything concerning or if adjustments are not improving your scores
This loop gives you a systematic method rather than random guessing. Small shifts add up to significant improvements.
The First 7 Nights Plan: Install Your Routine
Lock One Pre-Bed Cue
Choose a single action that happens at the same time every night. Effective cues include brushing your teeth, placing your phone on a charger in another room, or changing into sleep clothes.
The cue triggers medication time. No decisions required. No mental calculation about whether tonight feels like the right moment. The cue happens, you take your dose, and your wind-down begins.
Repeat a 20–30 Minute Wind-Down
After taking your medication, spend 20–30 minutes in dim light doing something calming. Reading a physical book works well. Gentle stretching works. Listening to quiet music works.
What does not work: scrolling your phone, checking email one last time, or watching intense television. These activities fight against the medication’s effects.
The wind-down period allows the medication to begin working while you help your brain transition toward sleep.
What to Log Nightly
Keep a simple record on paper or in a notes app:
- Dose time: When you took your medication
- Bedtime: When you actually got into bed
- Wake time: When you woke up
- Clarity score: Your 1–10 rating
- Notes: Anything unusual (stress, late meal, travel)
This log becomes invaluable when discussing your progress with your clinician. Patterns that feel invisible day-to-day become obvious when you review a week of data.
When to Message Your Clinician
Reach out through your patient portal if you experience any of the following:
- Clarity scores below 5 for three consecutive mornings despite timing adjustments
- Unusual symptoms like sleepwalking, confusion, or memory gaps
- Persistent difficulty falling asleep even with medication
- Significant mood changes
These situations warrant clinical input rather than continued self-adjustment. Your clinician can evaluate whether a dosage change, medication switch, or additional assessment makes sense.
What to Avoid Near Your Dose for Best Results
A few simple guidelines help your medication work as intended and protect your morning clarity.
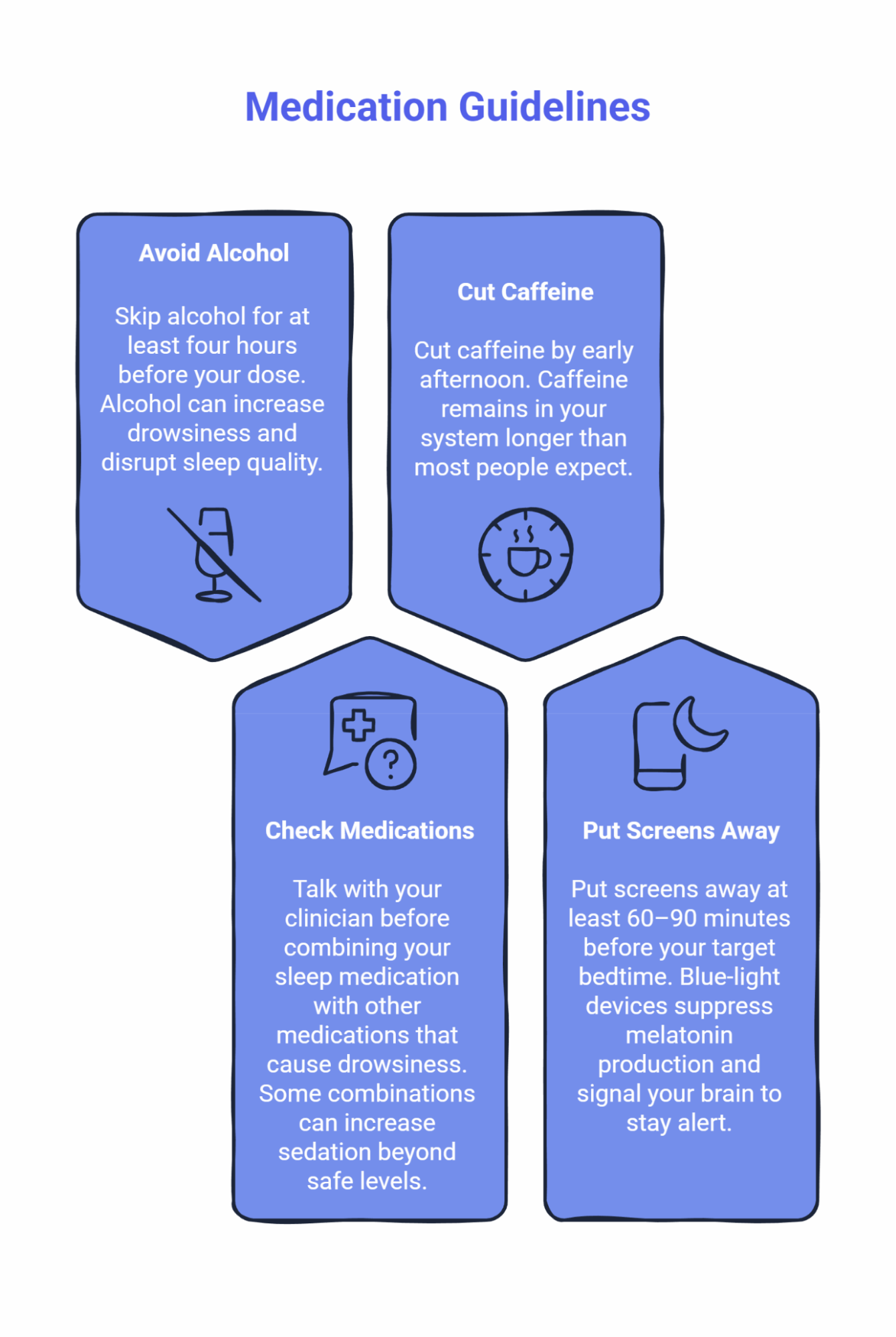
Skip Alcohol Before Bed
Avoid alcohol for at least four hours before your dose. Alcohol can increase drowsiness beyond what your medication alone produces, and it disrupts the quality of your sleep. Your medication works better when alcohol is not in the mix.
Check With Your Provider About Other Medications
If you take other medications that cause drowsiness—including certain antihistamines, muscle relaxants, or anxiety medications—talk with your clinician before combining them with your sleep medication. Some combinations can increase sedation beyond safe levels, so your provider needs to know your complete medication list.
Cut Caffeine by Early Afternoon
Caffeine remains in your system longer than most people expect. The Sleep Foundation notes that caffeine’s half-life ranges from 3–7 hours depending on individual metabolism. A 2 PM cutoff works for most people, though some may need to stop earlier.
Put Screens Away Before Bed
Blue-light devices (phones, tablets, computers) suppress melatonin production and signal your brain to stay alert. Put screens away at least 60–90 minutes before your target bedtime. If you must use devices, enable night mode settings that reduce blue light emission.
For a complete breakdown, read What to Avoid to Prevent Morning Grogginess.
Travel and DST: Keep the Window When the Clock Moves
Time zone changes and Daylight Saving Time transitions disrupt even well-established medication routines. The key principle: shift gradually toward your destination bedtime rather than making abrupt jumps.
Eastbound vs. Westbound Adjustments
Direction | Adjustment Strategy | Example |
|---|---|---|
Eastbound (losing hours) | Shift dose 30–60 min earlier each night for 2–3 nights before travel | NYC to London: Start shifting 3 nights before departure |
Westbound (gaining hours) | Shift dose 30–60 min later each night for 2–3 nights before travel | LA to Tokyo: Start shifting 3 nights before departure |
The goal is reaching your destination with a medication schedule already aligned to local time. This prevents the double disruption of jet lag plus medication mistiming.
Daylight Saving Time (March and November)
DST creates a one-hour shift twice yearly. In March, clocks spring forward, effectively making your medication feel like it comes an hour later relative to sunrise. In November, clocks fall back, making your dose feel an hour earlier.
For the week surrounding each transition, shift your dose by 15–20 minutes every other night until you reach the new clock time. This gradual approach prevents the grogginess spike that accompanies abrupt changes.
Understanding Your Care Options: Asynchronous vs. Video Visit
SleepScriptMD offers care across the USA, and the specific process depends on your state’s telehealth regulations and your individual clinical needs.
The typical care pathway flows like this: Intake → Clinician Review (or Video Visit if Required) → Prescription to Your Pharmacy → First Week Check-Ins
Asynchronous Care (Where Permitted)
In many cases, you can complete an online intake, a licensed clinician reviews your information, and your prescription goes to your pharmacy—often the same day. No video appointment required in these situations.
This streamlined approach works when your medical history and sleep concerns fall within straightforward parameters that allow for safe remote assessment.
Video Visit Care (When Required)
Some situations require a brief video visit before prescribing. This may be due to your state’s specific telehealth laws or because your clinical situation benefits from a real-time conversation with your provider.
Video visits typically last 10–20 minutes and cover your sleep history, current symptoms, and treatment goals. These sessions ensure your provider has all the information needed to create a safe, effective treatment plan.
How You’ll Know Which Applies to You
When you begin your intake, the system will guide you based on your location and responses. You’ll know immediately whether you can proceed with asynchronous care or need to schedule a brief video visit.
Regardless of the format, licensed clinician review is always part of your care. No prescriptions are auto-generated without physician oversight.
To see how care delivery works in your specific situation, visit the pricing page or compare AI-assisted vs. virtual care options in detail.
Safety First: Eligibility and When to Seek In-Person Care
Physician-guided online sleep treatment works well for many people, but it is not appropriate for everyone. Understanding eligibility helps you determine whether this path fits your situation.
Who Qualifies
You may be eligible if you meet all of the following:
- Between 18 and 65 years old
- No major medical conditions that could make sleep medications unsafe
- No active severe mental health conditions
- No current substance use disorders
- Not pregnant and not planning to become pregnant
If you have questions about a specific situation, reach out to admin@sleepscriptmd.com.
Sleep Apnea Screening
If you snore loudly, gasp during sleep, or have been told you stop breathing at night, you may need an at-home sleep test before starting medication. Obstructive sleep apnea requires different treatment approaches, and certain sleep medications can worsen apnea symptoms.
SleepScriptMD can help arrange at-home sleep testing if screening suggests this need.
Conditions That Require In-Person Evaluation
Some sleep disorders cannot be safely evaluated or treated through telehealth. If you experience any of the following, please seek evaluation from a local sleep specialist or neurologist:
Possible Narcolepsy Signs:
- Falling asleep unexpectedly during activities like talking or driving
- Sudden muscle weakness during strong emotions (knees buckling when laughing)
- Feeling paralyzed when falling asleep or waking up
REM Sleep Behavior Disorder Signs:
- Physically acting out dreams (yelling, kicking, punching during sleep)
- Your bed partner reports you move violently during sleep
Restless Legs Syndrome:
- Uncomfortable urge to move your legs at night or while resting
- Symptoms that worsen in the evening and improve with movement
These conditions require specialized testing and evaluation that online platforms cannot provide. The Narcolepsy Network Resource Center offers support for those exploring a narcolepsy diagnosis.
Additional Resources
For readers seeking deeper context on sleep health and sleep disorders research, the National Heart, Lung, and Blood Institute’s National Center on Sleep Disorders Research provides comprehensive, evidence-based information on sleep science and sleep medicine.
Frequently Asked Questions
How consistent should I keep my timing window in week one?
Aim for the same 30-minute window every single night. Consistency during the first week establishes baseline data and allows your body to develop a predictable response pattern.
What should I do if my clarity score stays under 7?
First, try shifting your dose 15–30 minutes earlier for two consecutive nights. If scores remain low after timing adjustments, message your clinician through the patient portal for guidance.
Is alcohol safe near my dose?
No. Avoid alcohol for at least four hours before taking your sleep medication. Alcohol disrupts sleep quality and can increase drowsiness beyond what your medication alone produces.
How do I adjust timing for a new time zone?
Shift gradually. Move your dose 30–60 minutes toward your destination bedtime each night for 2–3 nights before travel. This allows smoother adjustment than abrupt changes upon arrival.
When is a video visit required before prescribing?
Whether you proceed with asynchronous care or need a video visit depends on your state’s telehealth regulations and your individual clinical situation. The intake process will let you know which approach applies to you. Check the pricing page for more details.
What if I snore or gasp during sleep?
You may need an at-home sleep test before starting medication to rule out obstructive sleep apnea. Mention this during intake so your clinician can arrange appropriate screening.
Your Next Steps
Getting started takes just a few minutes. Choose the path that matches your readiness:
Not sure if you need help? Take the 6-Second Sleep Check for a quick gut check, or try the Sleep Clarity Quiz for more detailed insights. The Deep Sleep Profiler provides the most comprehensive screening if you want thorough answers.
Ready to start treatment? Start your sleep treatment to begin your intake. Same-day prescriptions are often available where asynchronous care is permitted. Your first month costs just $25, with no hidden fees and the freedom to cancel anytime.
Want to learn more about your options? Explore our treatments offered to understand which non-addictive medications might work for your sleep pattern, or review pricing to see what fits your budget.
Have questions about whether this approach fits your situation? Contact the team at 1-800-RESTFUL or hope@sleepscriptmd.com.
Clear mornings start with the right timing. Lock your window tonight.
Disclaimer: This content is educational and does not constitute medical advice, diagnosis, or treatment. Always follow your clinician’s specific guidance regarding medication timing and dosage. Individual responses to sleep medications vary, and the timing suggestions provided here represent general starting points rather than personalized medical recommendations.
