Key Takeaways
Key Takeaways
Morning grogginess after taking sleep medication doesn’t have to be your reality.
- Three Evening Rules Change Everything: Stopping alcohol 3-4 hours before bed, cutting caffeine by early afternoon, and avoiding screens 60-90 minutes before sleep creates the conditions for your medication to work as intended and your mind to wake up clear.
- Timing Trumps Dosage: Taking your prescribed sleep medication at a consistent time every night—paired with these three avoidance strategies—helps your body establish a rhythm that supports both quality sleep and sharp morning function.
- Track Your Clarity Score: Rating your mental sharpness each morning (1-10 scale) within 30 minutes of waking gives you objective feedback on whether your routine is working, with scores of 7+ indicating optimal results.
- Interactions Extend Beyond the Obvious: Combining your prescription with alcohol, late caffeine, over-the-counter sedatives, or blue light exposure doesn’t just delay sleep—it can amplify sedative effects and extend grogginess well into your morning hours.
- Provider Partnership Accelerates Results: When persistent grogginess occurs despite following guidelines, a simple 15-30 minute adjustment to your medication timing—discussed with your provider—often resolves the issue within 3-4 days.
Patients using trazodone, hydroxyzine, or clonidine for insomnia will find practical strategies here, preparing them for the detailed guidance that follows.
You took the first step. You talked to a physician, got a prescription for a non-controlled sleep medication, and you’re finally addressing those restless nights. Now you want to make sure you wake up clear and ready to go.
Picture this: It’s 6:30 a.m., your alarm is blaring, and you have an important presentation at 9:00. You reach for your phone and feel sharp, focused, ready. This is what you’re working toward when you’re using your prescribed sleep medication correctly.
Here’s what makes the difference: non-controlled sleep medications like trazodone, hydroxyzine, and clonidine are commonly prescribed options for sleep difficulties. These medications are not habit-forming like controlled substances, and when used under physician supervision, they can help you fall asleep and stay asleep. Many are prescribed off-label for insomnia, meaning they’re used for sleep even though they were originally developed for other conditions.
The key to waking up clear? Three simple evening habits. When you avoid alcohol close to bedtime, cut off caffeine by early afternoon, and give yourself a break from screens before bed, you’re creating the conditions that allow these medications to work as your doctor intended.
Why These Three Rules Matter
When physicians prescribe non-addictive sleep medications, they’re giving you tools to address persistent sleep difficulties. These medications—whether you’re taking trazodone, which increases time spent in deep sleep stages, hydroxyzine for its sedating effects, or clonidine to reduce nervous system activity—work through specific effects on brain chemistry to promote sleep onset and maintenance.
Consistent timing supports better mornings. When you take your medication at a regular time and follow basic evening guidelines, you’re setting yourself up for sleep followed by a clearer, more functional morning.
Your avoid list protects results. Three common evening habits—alcohol consumption, late caffeine intake, and blue-light device exposure—can interfere with your medication’s effectiveness. They either extend how long the medication stays active in your system, delay your ability to fall asleep, or disrupt your sleep quality so you wake up feeling unrefreshed despite adequate hours in bed.
Understanding these interactions helps you get the most from your treatment. These aren’t complicated restrictions—they’re straightforward habits that support your prescribed sleep plan.
The Three Rules for Clear Mornings
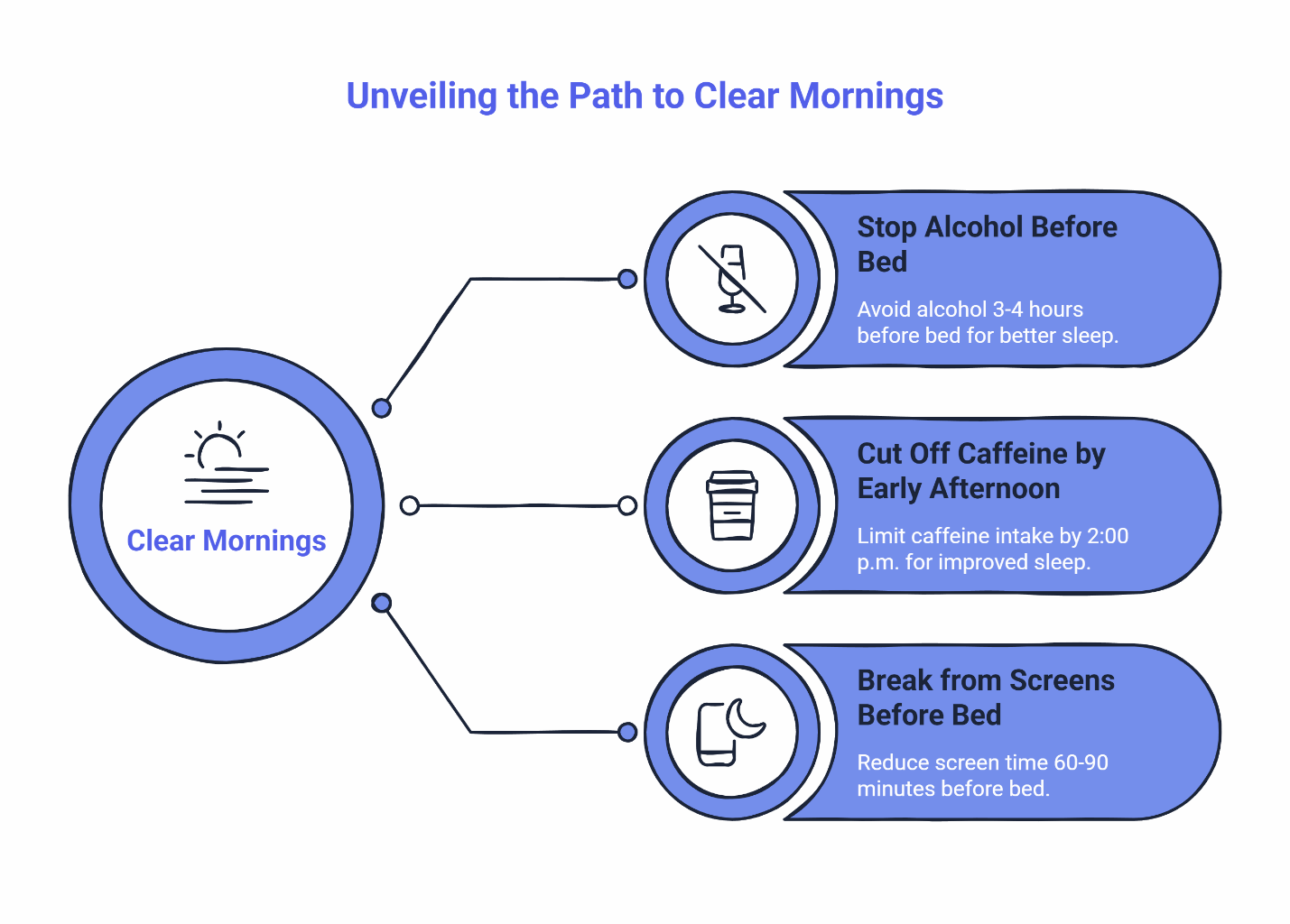
Stop Alcohol Three to Four Hours Before Bed
Both alcohol and your sleep medication are central nervous system depressants. When you combine them, the sedative effects are amplified, which can extend into the next morning and affect your clarity.
There’s another issue: alcohol disrupts your sleep architecture. It interferes with REM sleep and causes more frequent awakenings in the second half of the night, as noted in guidance from Johns Hopkins Medicine on good sleep habits. Even though you might fall asleep faster, the quality of that sleep is reduced—and your medication can’t compensate for that disruption.
The guideline: Stop drinking alcohol at least three to four hours before you take your medication or go to bed. If you take your medication at 10:00 p.m., your last drink should be around 6:00 or 7:00 p.m.
Practical tip: Set a reminder on your phone if you’re out with friends or attending an evening event. This simple step protects tomorrow morning’s clarity.
Important note: Avoid combining your sleep medication with other sedating products, including over-the-counter antihistamines. If you’re considering any new medications or supplements, check with your provider first.
Cut Off Caffeine by Early Afternoon
Caffeine has a half-life of about three to five hours in most adults, but its effects can linger longer. When you consume caffeine late in the day, you’re delaying sleep onset and potentially reducing how well your medication works.
Here’s why: caffeine blocks adenosine receptors in your brain. Adenosine is the chemical that builds up during the day and makes you feel sleepy. Your sleep medication works most effectively when your body’s natural sleep pressure is high. When caffeine is still blocking those receptors, your medication has to work harder.
Research shows that consuming caffeine even six hours before bed can reduce total sleep time and worsen sleep quality. A 4:00 p.m. coffee can still be affecting your sleep at 10:00 p.m. This is why MedlinePlus guidance on healthy sleep recommends avoiding caffeine in the afternoon and evening.
The guideline: Aim to stop caffeine intake by 2:00 p.m. If you’re sensitive to caffeine, consider moving that cut-off to noon or 1:00 p.m.
Watch for hidden sources: Caffeine isn’t just in coffee. Tea, energy drinks, certain sodas, chocolate, and some over-the-counter pain relievers all contain caffeine. Check labels in the afternoon and evening.
Alternative pick-me-ups: Try a short walk, cold water, or a healthy snack instead. These won’t interfere with your evening medication.
Give Yourself a Break from Screens Before Bed
Blue light from phones, tablets, computers, and televisions suppresses melatonin production and shifts your circadian rhythm. When you’re using devices right up until you take your sleep medication, you’re signaling to your brain that it’s still daytime.
Blue light exposure in the evening can delay REM sleep onset and reduce sleep quality, as explained by Stanford Medicine researchers studying blue light’s impact. Your medication helps you fall asleep, but if your internal clock is confused, the quality of that sleep—and how you feel the next morning—may be affected.
The guideline: Put devices away sixty to ninety minutes before bed. If you take your medication at 10:00 p.m., aim to finish screen time by 8:30 or 9:00 p.m.
If you must use devices: Enable warm light modes (often called “night shift” or “blue light filter”) on all screens. Dim your brightness and keep devices farther from your eyes to reduce light intensity. These adjustments help minimize the disruption.
Better alternatives: Use the hour before bed for screen-free activities—reading a physical book, gentle stretching, preparing tomorrow’s clothes, or talking with family. These support your body’s wind-down process.
Track Your Morning Clarity
Numbers help you see what’s working. That’s why tracking your morning clarity gives you feedback about whether your timing and evening routine are on track.
How to Score Your Mornings
Each morning within thirty minutes of waking, rate your mental clarity on a scale of one to ten:
- 1-3: Severe grogginess—difficulty forming thoughts or managing basic tasks
- 4-6: Moderate grogginess—functional but noticeably slower than usual
- 7-8: Good clarity—alert and capable with minimal transition time
- 9-10: Excellent clarity—refreshed and sharp, ready to start immediately
Your goal is to consistently score seven or higher. This suggests your medication timing and evening routine are working well together.
If Your Score Stays Below Seven
Before assuming the medication isn’t right, consider adjusting your timing. A simple shift of fifteen to thirty minutes earlier or later often makes a difference.
Work with your provider on this. Report your clarity scores and discuss whether changing your medication time might help. After making a timing adjustment, track your scores for three to four days to see if it improves your mornings.
Keep a simple log: date, medication time, morning clarity score, and any deviations from your avoid list. This helps you and your provider identify patterns.
Other Factors That Can Affect Morning Clarity
A few additional factors can interfere with clear mornings:
Heavy late dinners—especially high-fat meals—force your digestive system to work when it should be winding down. Aim to finish dinner two to three hours before bed.
Sedating over-the-counter medications can amplify your prescription medication’s effects. Diphenhydramine (in many allergy and sleep aids) and certain pain relievers with sedating ingredients should be discussed with your provider before use.
Long evening naps reduce your sleep pressure right when you need it high. Keep naps short, earlier in the day, and away from your bedtime window.
When to Reach Out to Your Provider
Most people find these medications can work well once timing and evening habits are in place. Contact your provider if:
- You experience persistent next-day grogginess despite following these guidelines for several days
- You develop new symptoms that concern you
- Your clarity score stays below seven for more than a week despite adjustments
For non-urgent questions, use your returning patient portal to message your care team. They can help you fine-tune your approach.
Pair Your Medication with Consistent Timing
These evening habits work best when combined with a consistent medication schedule. Taking your prescription at roughly the same time every night helps your body establish a rhythm. Your sleep pressure peaks at the right moment, your medication reaches optimal levels at the right time, and your wake-up aligns with when it has cleared your system.
Ready to get started with physician-supervised sleep care? Start your confidential assessment or explore which medications we offer.
Quick-Reference Checklist: What to Avoid for Clear Mornings
Alcohol
- Stop: 3-4 hours before bed or medication
- Why: Disrupts sleep quality and extends sedative effects
- Tip: Set a phone reminder
Caffeine
- Stop: By 2:00 p.m. (earlier if sensitive)
- Why: Delays sleep onset and may reduce medication effectiveness
- Tip: Switch to decaf or water after lunch
Devices (Blue Light)
- Stop: 60-90 minutes before bed
- Why: Suppresses melatonin and delays sleep timing
- Tip: Use warm screen modes if needed; keep farther from eyes
Clarity reminder: If your morning score stays below 7 for two or more days, discuss a 15-30 minute timing adjustment with your provider and track for 3-4 days.
Simple Guidelines, Better Sleep
When you follow these three straightforward rules—stopping alcohol three to four hours before bed, cutting off caffeine by early afternoon, and taking a break from screens in the evening—you’re creating conditions that support your prescribed sleep medication.
These aren’t complicated medical protocols. They’re practical habits that help you get the most from your treatment. When you combine them with consistent timing and work with your provider to fine-tune your approach, you create a pattern that supports better sleep and clearer mornings.
Important Information
This article is for educational purposes only. Non-controlled sleep medications should be used under the supervision of a licensed healthcare provider. Individual responses to medications vary. Content reflects guidance for low-risk adults ages 18-65. If you’re pregnant, trying to conceive, or outside this age range, or if you have conditions that may require in-person evaluation (such as suspected narcolepsy, REM sleep behavior disorder, or active restless legs syndrome), please visit Getting Started for guidance. Some states require a brief virtual visit before prescribing; availability and process may vary by location.
Our Editorial Process
The SleepScriptMD Insights Team creates evidence-based content to help patients understand sleep health and treatment options. Our articles are developed using peer-reviewed research, clinical guidelines, and input from licensed medical professionals. All content undergoes review for accuracy and clarity before publication.
About the SleepScriptMD Insights Team
Our editorial team combines expertise in sleep medicine, psychiatry, and patient education to deliver practical, trustworthy guidance. We focus on translating complex medical information into actionable advice that supports informed decision-making about sleep health.