📌 Key Takeaways
Morning grogginess from travel isn’t your medication failing—it’s your timing needing a 30–60 minute shift per night toward your destination bedtime.
- Shift Before You Fly: Adjust your dose 30–60 minutes earlier (eastbound) or later (westbound) starting two nights before departure.
- Commit to One Clock: Take your medication at destination bedtime once you’re sleeping on the plane, not your origin time.
- Score Your Mornings: Rate clarity 1–10 each day; below 7 means nudge timing 15–30 minutes the next night.
- Protect Your Window: Skip alcohol 3–4 hours before dosing and cut caffeine by early afternoon for cleaner wake-ups.
- DST Prep Prevents Fog: Move your dose 15–30 minutes earlier per night for 2–3 nights before spring-forward transitions.
Gradual shifts beat dramatic changes—your body adjusts when timing stays consistent.
Adults managing insomnia with non-controlled medications will find travel-ready protocols here, preparing them for the detailed timing planner and scenario examples that follow.
You’re packing for a big trip. The flight leaves early, and you’ve got a crucial meeting the morning after you land. Your non-controlled sleep medication works perfectly at home. But crossing time zones? That’s where things get tricky.
Here’s the good news: these medications are designed to work with your schedule, not against it. When you anchor your dose to your destination bedtime and shift gradually, you protect both your sleep and your next-day clarity. This guide gives you a concrete plan you can screenshot tonight and use on every trip.
Quick Answer: Shift by 30–60 Minutes Toward Destination Bedtime
- Shift your dose toward your target destination bedtime by 30–60 minutes per night across travel days.
- On the plane, switch to the destination clock once you commit to sleep.
- Use your 1–10 Morning Clarity Score to fine-tune timing the next night.
Not sure if your sleep issues need medication? Take our 6-Second Sleep Check for a quick assessment, or try the 2-Minute Sleep Clarity Quiz for personalized guidance.
Why Timing Matters When You Travel
Your body’s internal clock doesn’t reset the moment you land somewhere new. Research from the American Academy of Sleep Medicine confirms that abrupt schedule changes can worsen next-morning grogginess. The solution isn’t skipping your medication or doubling down on it. The solution is simple timing adjustments.
Your internal clock responds to cues like light, darkness, and meals. The National Institute of General Medical Sciences explains that these biological patterns regulate everything from hormone release to body temperature throughout the day. Crossing time zones scrambles those cues, which is why you can feel sleepy at the wrong time or wide awake at bedtime.
Non-controlled sleep medications like trazodone, hydroxyzine, and clonidine work best when taken consistently at the same relative time each night. These medications are not controlled substances and are not habit-forming like benzodiazepines or sleep aids such as Ambien. When taken as prescribed under medical supervision, they offer flexibility for travelers. Maintaining consistency relative to your destination schedule helps your body get the stability it needs while your internal clock catches up naturally.
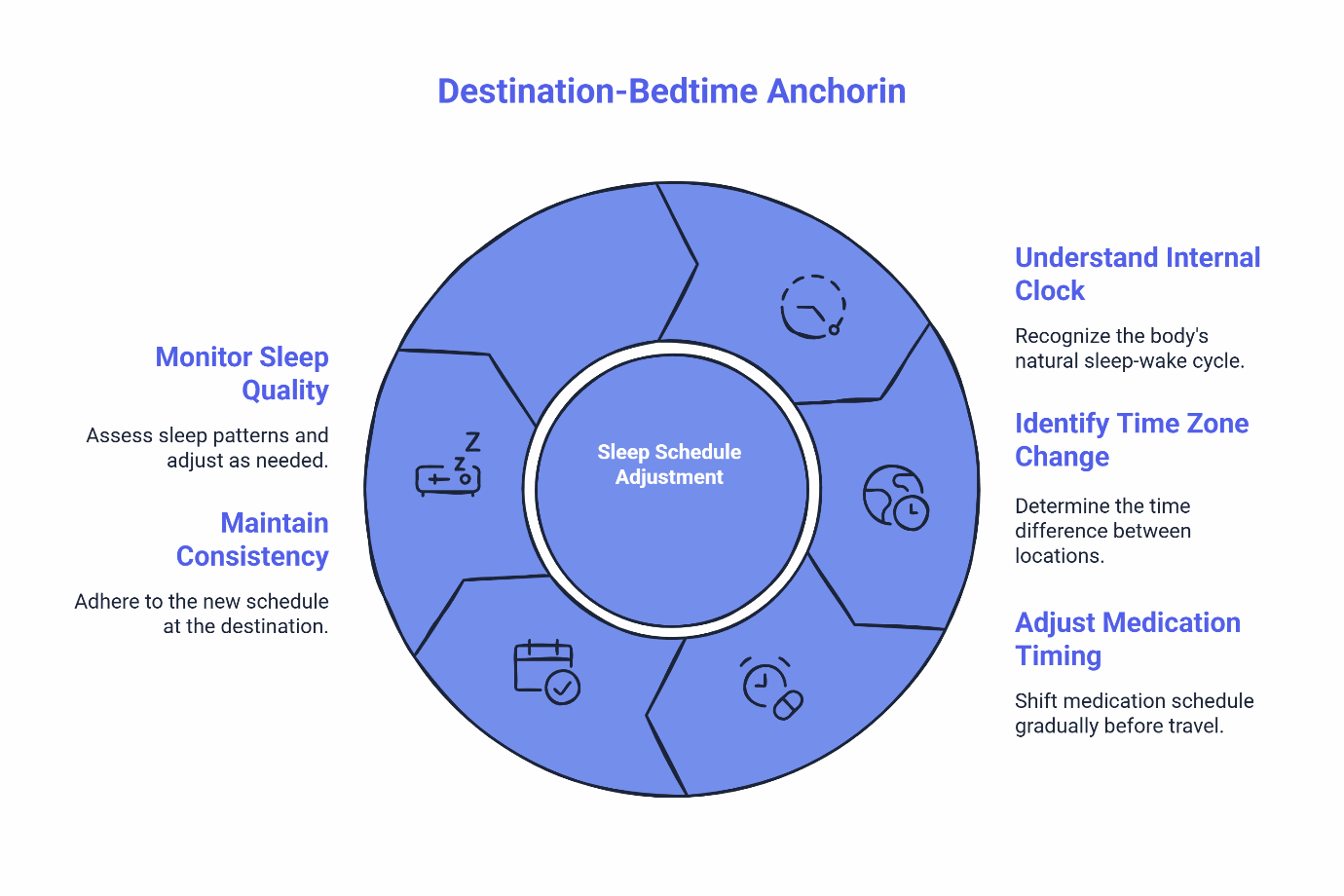
Destination-bedtime anchoring means you start shifting your dose before you leave, aligning gradually with where you’re going rather than where you are. This straightforward approach reduces the mismatch that causes that foggy feeling after crossing multiple time zones. For more on how these medications work and why timing matters, see our Treatments Offered page.
Your Travel Timing Planner (Save or Screenshot)
This table gives you night-by-night guidance based on your direction of travel and the size of your time zone shift. The rule is simple: shift 30–60 minutes per night toward your destination bedtime.
Time Zone Shift | Direction | Night −2 | Night −1 | Travel Night | Night +1 | Expected AM Feel | Clarity Rule |
|---|---|---|---|---|---|---|---|
1–3 hours | East | 30 min earlier | 30 min earlier | Destination bedtime | Hold | Mild adjustment | If <7, shift 15 min earlier |
1–3 hours | West | 30 min later | 30 min later | Destination bedtime | Hold | Mild adjustment | If <7, shift 15 min later |
4–6 hours | East | 45 min earlier | 45 min earlier | Destination bedtime | Hold or 30 min earlier | Moderate adjustment | If <7, shift 15–30 min earlier |
4–6 hours | West | 45 min later | 45 min later | Destination bedtime | Hold or 30 min later | Moderate adjustment | If <7, shift 15–30 min later |
7–8+ hours | East/West | 60 min shift | 60 min shift | Destination bedtime | Fine-tune based on clarity | Expect 2–3 days adjustment | Use clarity score daily |
The Clarity Adjustment Loop: If your Morning Clarity Score falls below 7 the next day, nudge your dose 15–30 minutes earlier (when traveling east) or later (when traveling west) the following night. Small adjustments compound into smoother transitions.
Safe Travel with Your Sleep Medication
Your medication is designed to be flexible. These non-controlled medications work reliably when you maintain consistent timing relative to your destination. Most people adjust smoothly within 2–3 days using the planner above.
Service eligibility: This guide applies to adults who meet SleepScriptMD’s eligibility criteria, which may include age restrictions (often 18–65) and medical history considerations that vary by state and regulatory requirements. Individual health factors determine whether these medications are appropriate, and medical supervision is required. If you experience symptoms suggesting narcolepsy, REM sleep behavior disorder, or significant restless legs syndrome, please seek in-person evaluation with a local sleep specialist, as these conditions require testing that virtual care cannot provide.
State variations: Telemedicine regulations differ by jurisdiction. Some states require a brief virtual visit before prescribing. Check our AI-Assisted vs Virtual Appointments page for your state’s pathway.
Morning Clarity Self-Check (1–10)
Rate yourself each morning during your trip:
- 9–10: Clear head, no lingering drowsiness. Your timing is working perfectly.
- 7–8: Slightly slower for the first 60–90 minutes. Acceptable for most people.
- 5–6: Noticeable grogginess. Adjust timing by 15–30 minutes next dose.
- ≤4: More drowsiness than expected. Message your clinician through our Returning Patients portal.
This simple rubric lets you fine-tune your approach within a few nights rather than guessing through an entire trip.
Plane-Day Tactics
Red-Eye Flights: If you plan to sleep on the plane, take your medication at your destination bedtime (even if that feels early by your origin clock). Commit fully to the destination schedule once you decide to sleep. Reducing bright light exposure as you approach your sleep window helps because light influences your internal clock.
Daytime Flights: Skip your sleep medication during daytime travel. Save your dose for actual bedtime at your destination. Taking medication during a daytime flight can leave you drowsy on arrival with no recovery time before evening.
Layovers: Treat the entire trip as one continuous “travel night.” Keep the same destination bedtime target throughout. Avoid stacking multiple sleep attempts across connections. If sleep happens during a layover, keep it short and intentional rather than forcing a full sleep cycle.
Handling Missed Windows: If you miss your target dosing window by more than two hours, it’s generally better to skip that dose and reset the next night. Taking a sleep aid too late can push drowsiness into your morning. When in doubt, message your clinician through the Returning Patients portal.
Naps: Keep them short. A 20–30 minute nap early in the afternoon won’t derail your evening dose timing. Longer naps or late-afternoon sleep can make it harder to fall asleep at your target bedtime.
Stay hydrated throughout your flight. Dehydration makes fatigue worse and can affect how you feel the next morning. Minimize caffeine after early afternoon, especially on travel days.
DST Cheat Sheet (USA)
The American Academy of Sleep Medicine has documented that clock changes can disrupt sleep due to the mismatch between your schedule and your body’s natural rhythm. Even a one-hour shift can affect your sleep when you’re relying on timed medication.
Daylight Saving Time transitions happen on the second Sunday of March (spring forward) and November (fall back).
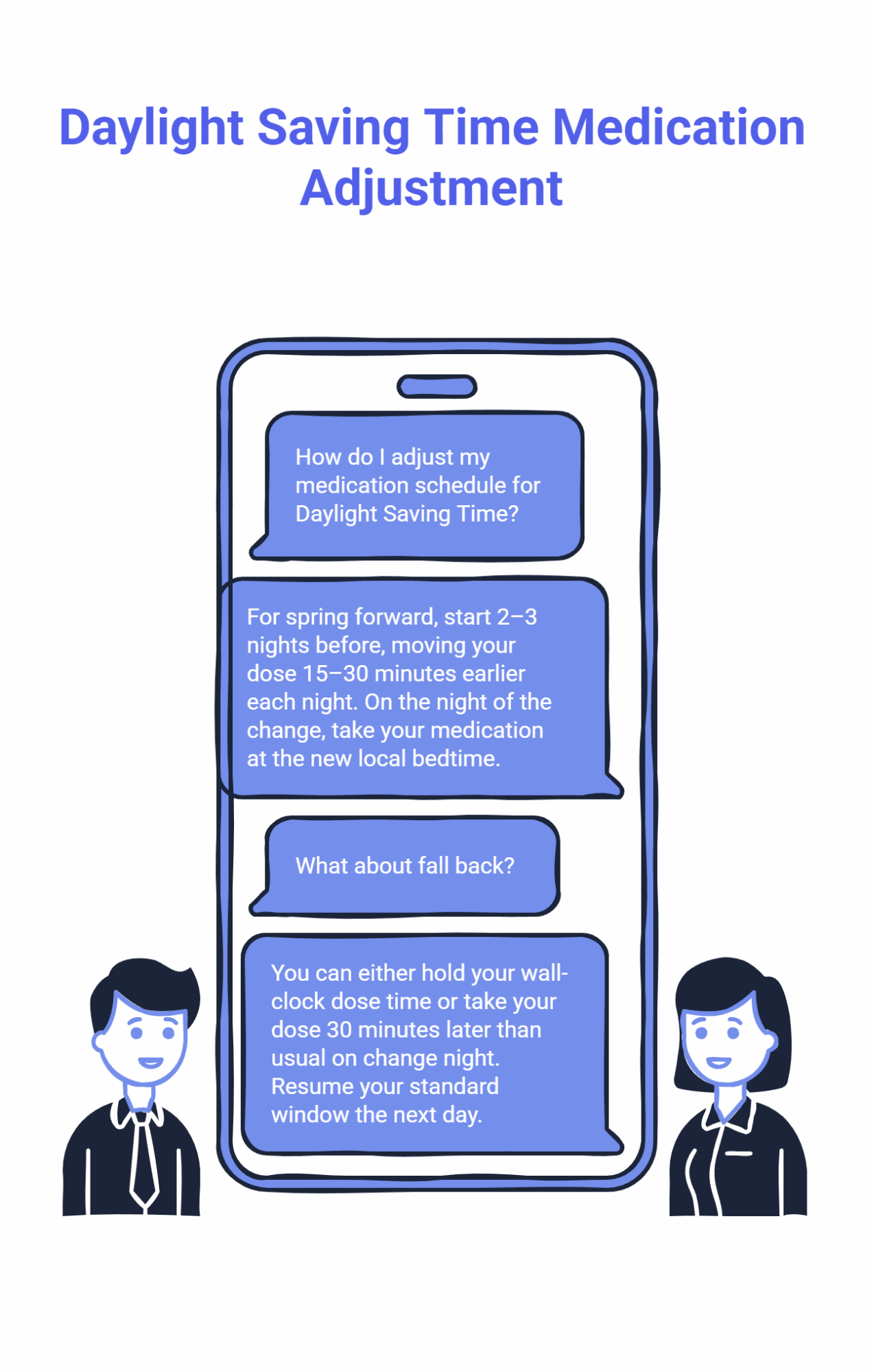
Spring Forward (March):
Start 2–3 nights before the change. Move your dose 15–30 minutes earlier each night. On the night clocks change, take your medication at the new local bedtime. You’ll have pre-adjusted, so the transition feels minimal.
Fall Back (November):
This one’s easier. You can either hold your wall-clock dose time (which means your body experiences an extra hour before medication) or split the difference by taking your dose 30 minutes later than usual on change night. Resume your standard window the next day.
The key insight: DST affects everyone, but it’s easier to manage when you prepare a few nights ahead. A little planning prevents the grogginess that catches most people off guard. For more on seasonal sleep disruptions, see our FAQs.
Simple Guidelines for Better Travel Sleep
Following these straightforward practices helps your medication work its best while traveling:
Alcohol: Avoid drinking within 3–4 hours of your planned dose. The CDC recommends avoiding alcohol for at least four hours before bedtime because it can affect sleep quality and how you feel the next morning.
Caffeine: Cut off caffeine by early afternoon. The CDC notes that stopping caffeine at least 5–6 hours before sleep supports better rest. During time zone shifts, your body is already adjusting. Avoid adding stimulants to the mix.
Screens and Light: Wind down 60–90 minutes before your target bedtime. Blue light delays natural drowsiness, and the CDC recommends limiting light exposure before sleep. This matters more during transitions when your schedule is already off-balance.
For a complete checklist and additional guidance, visit our FAQs page.
Copy-and-Paste Scenarios
NYC → London (5 hours east): You normally take your medication at 10 PM. Start shifting two nights before departure: Night −2 at 9 PM, Night −1 at 8 PM. On your travel night (likely a red-eye), take it at 10 PM London time, which is 5 PM New York time. This shift works smoothly because you’re committing to sleep on the plane. Land, push through to London evening, dose at 10 PM local. Expect a clarity score around 6–7 the first morning. Adjust by 15–30 minutes if needed.
SF → NYC (3 hours east): Your usual 11 PM dose shifts to 10:30 PM two nights before, then 10 PM the night before travel. On arrival in New York, dose at 11 PM Eastern. This is a gentler transition. Most people score 7–8 on clarity the first morning with no further adjustment needed.
Chicago → Hawaii (4 hours west): Going west is generally easier. Your 10 PM dose shifts later: 10:30 PM, then 11 PM over two nights. In Hawaii, dose at 10 PM local. Your body experiences this as staying up slightly later each night, which most people adapt to within one or two days.
When to Reach Out
Contact your clinician through the Returning Patients portal if you experience:
- Morning Clarity scores of 4 or below for two consecutive days
- Unexpected symptoms that weren’t present before travel
- Difficulty returning to your normal schedule within a week of returning home
- Any questions about adjusting your timing
Some states require a brief virtual visit for prescription adjustments. Check our AI-Assisted vs Virtual Appointments page for your state’s pathway and Pricing for fee details, including the 90-day prescription option.
Ready to Start Treatment with Non-Controlled Sleep Medications?
Travel doesn’t have to mean sacrificing sleep. With the right medication and simple timing adjustments, you can maintain consistent rest no matter where you’re headed.
SleepScriptMD offers physician-guided treatment with non-controlled medications like trazodone, hydroxyzine, and clonidine. These options are not habit-forming like controlled substances and are generally well-tolerated when taken as prescribed under medical supervision. Individual responses vary, so ongoing clinician guidance ensures the best outcomes.
Our asynchronous pathway (available in most states) gets you started quickly, often with same-day prescriptions where eligible. States requiring a brief virtual visit can typically schedule within a few days.
Start Your Sleep Treatment – Get Started Today
Compare your options on our AI-Assisted vs Virtual Appointments page, explore our non-controlled medication options, or review Pricing to understand what’s included.
Eligibility considerations: SleepScriptMD’s service criteria typically include age ranges (often 18–65) and medical history factors, which may vary based on state telemedicine regulations and individual health circumstances. Medical supervision is required to determine appropriateness. If you’ve been told you snore, gasp, or stop breathing during sleep, we can still help after you complete an at-home sleep test.
Disclaimer: This guide is educational and not a substitute for medical advice. Use only as directed by your clinician. For questions about your specific situation, visit our FAQs or Getting Started page.
