📌 Key Takeaways
Non-controlled prescription sleep medications work reliably when matched to your specific insomnia pattern and taken in consistent timing windows.
- Match Medication to Pattern: Clonidine calms racing thoughts, trazodone reduces nighttime awakenings, and hydroxyzine quiets anxiety-driven insomnia.
- Timing Beats Dose Adjustments: Taking your medication in the same 30-60 minute window each night prevents unpredictable morning grogginess.
- Track Your Morning Clarity Score: Rating alertness on a 1-10 scale guides small timing tweaks with your clinician before changing medications.
- Most Grogginess Is Clock Problems: Shifting your dose 15-30 minutes earlier resolves most morning fog without prescription changes.
- Avoid Evening Blockers: Skipping alcohol, cutting caffeine by 2 PM, and reducing screen time helps your medication work as intended.
Prepared timing + pattern-matched medication = predictable sleep and clear mornings.
Time-pressed adults seeking non-addictive prescription sleep solutions will gain a practical decision framework here, preparing them for the detailed implementation guide that follows.
From Late-Night Panic to Predictable Sleep
2:14 AM. The phone screen glows. You do the math again: if you fall asleep right now, you get four hours and twelve minutes. The presentation is at 9. Your brain won’t stop rehearsing the opening slide.
I can’t afford to be foggy tomorrow.
You’ve tried the melatonin. You’ve tried the blue-light-blocking glasses and the bedtime routine. You’ve read the sleep hygiene articles. And here you are, again, calculating sleep debt while your alarm creeps closer.
Here’s what changes: with the right non-controlled prescription sleep medication, matched to your specific insomnia pattern and taken in a consistent timing window, you can replace that 2 AM mental arithmetic with a predictable routine. You’ll use a simple 1-10 morning clarity score to fine-tune your timing during the first week, avoid the common evening blockers that sabotage treatment, and work with a clinician to install what many patients describe as “sleep auto-pilot.” This guide will show you the pattern-fit decision framework, the timing windows that protect your mornings, and the first-week playbook that replaces trial-and-error guessing.
The Foundation: What “Non-Controlled” Actually Means
Non-controlled sleep medications are supervised prescription options that help you sleep more predictably—whether your challenge is falling asleep, staying asleep, or shutting off a racing mind. These medications work through calming pathways in your nervous system, and when matched to your specific pattern and taken consistently, they can deliver the reliable sleep onset you need while keeping your mornings clear.
The term “non-controlled” means these medications aren’t classified as controlled substances by the DEA. They work through different mechanisms than benzodiazepines or Z-drugs—calming overactive nervous system signals, blocking histamine pathways that keep you alert, or enhancing deep sleep stages—without the dependency risks. Under clinician supervision, they provide the consistent sleep you need while protecting your next-day performance.
The goal isn’t to “knock you out.” It’s to install a predictable routine: choose the right fit, take it in a consistent timing window aligned to your target bedtime, avoid the common evening blockers (like alcohol, late caffeine, and bright screens), and track a simple 1-10 morning clarity score so you and your clinician can fine-tune without trial-and-error.
Quick Answer: When Non-Controlled Sleep Medications Make Sense
You might benefit from this supervised approach if you’ve been dealing with persistent insomnia despite good sleep habits and over-the-counter attempts, and you have a high priority on next-day clarity for work or life responsibilities. The pattern-fit framework works for people who are tired of the “just try this and see” cycle and want a more systematic path.
The supervised process emphasizes three things: a safety screen first (to confirm you’re a good candidate), matching the medication type to your specific insomnia pattern, and establishing timing windows that protect your morning performance. This isn’t about experimenting on your own—it’s about working with a clinician to find the right key for your specific lock.
You may not be a fit for this approach if:
- You’re under 18 or over 65
- You’re pregnant, planning pregnancy, or breastfeeding
- You have major medical, mental health, or substance use conditions that require closer monitoring
- You show signs of conditions that need in-person evaluation, such as falling asleep unexpectedly during the day, muscle weakness triggered by emotions, feeling paralyzed when waking, acting out dreams physically, or uncontrollable urges to move your legs at night
If any of those apply, a local sleep specialist or your primary care provider should evaluate you in person before starting treatment. For comprehensive details on what requires in-person care, review the eligibility criteria.
Step 1 — Identify Your Insomnia Pattern (Finding the Lock)
Before choosing a medication, you need to identify your specific pattern. Insomnia isn’t one condition—it’s three distinct patterns that respond to different approaches.
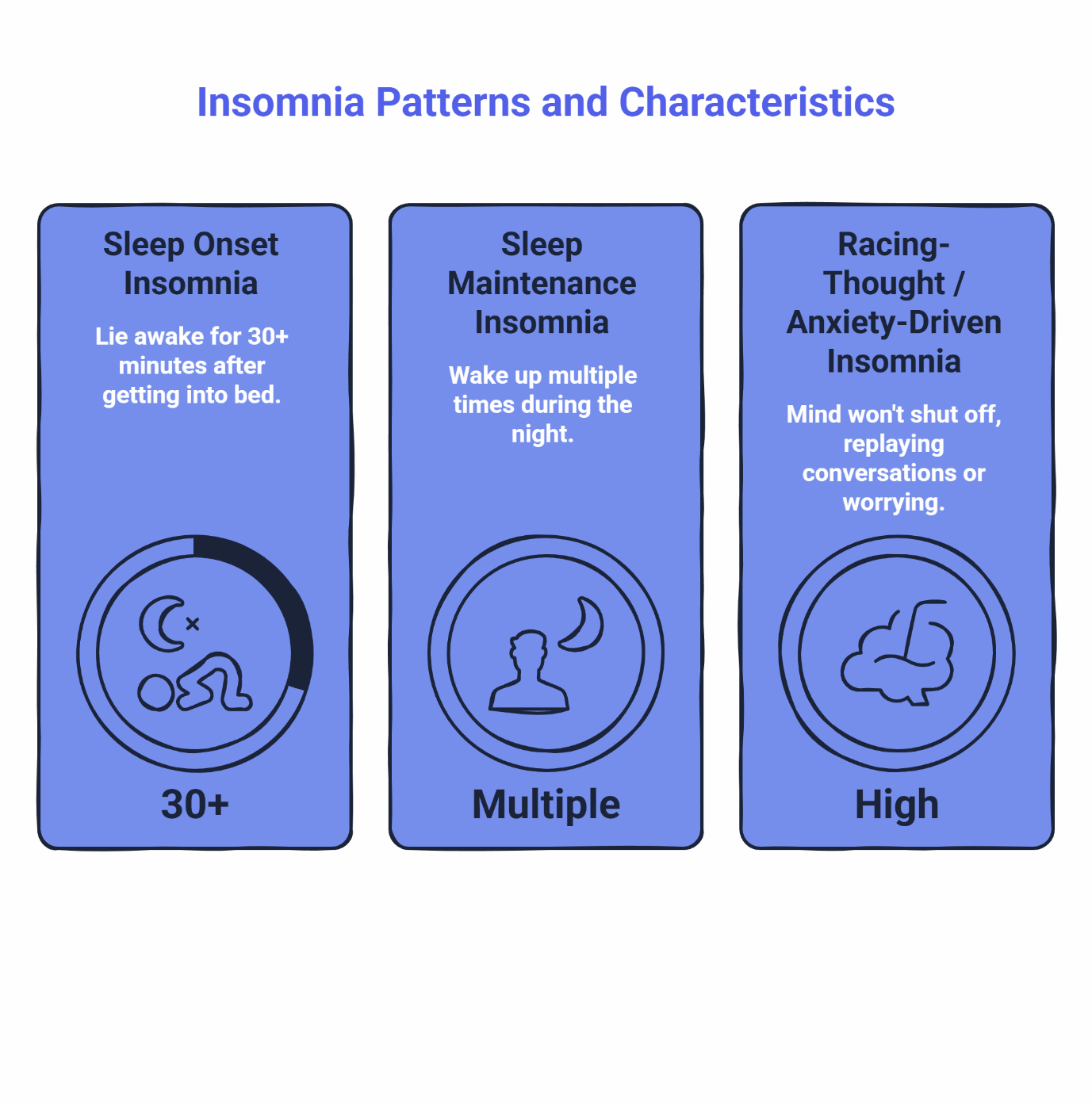
Sleep Onset Insomnia (Trouble Falling Asleep)
- You lie awake for 30 minutes or more after getting into bed
- Your mind races or you feel physically restless
- Once you finally fall asleep, you usually stay asleep
Sleep Maintenance Insomnia (Trouble Staying Asleep)
- You fall asleep within a reasonable time
- You wake up multiple times during the night and struggle to fall back asleep
- You may wake too early and can’t return to sleep
Racing-Thought / Anxiety-Driven Insomnia
- Your mind won’t shut off—you replay conversations, plan tomorrow, or worry
- Physical relaxation isn’t the problem; mental activation is
- You may have both onset and maintenance issues driven by the same anxious loop
Quick Self-Assessment:
Take twelve seconds right now and ask yourself:
- “When sleep fails, is the main problem the first 60-90 minutes—or the second half of the night?”
- “If the mind quieted down, would sleep come more easily?”
- “Is the main goal faster onset, fewer awakenings, or a calmer runway into bed?”
Which pattern describes your last three nights? That answer determines which medication type clinicians typically consider for your situation.
If your pattern keeps shifting night to night, track bedtime, timing, awakenings, and next-day clarity for one week using the Sleep Clarity Quiz before discussing options with a clinician.
Step 2 — The Medication Selection Matrix
These evidence-based, non-addictive medications can help you sleep more reliably when matched to your specific pattern. This table shows which options clinicians typically consider based on your insomnia type, along with what to expect for timing and morning clarity.
Remember: this is educational information to help you have an informed conversation with your clinician, not a prescription.
Your Pattern | What You’re Optimizing For | Safe, Non-Addictive Option | Expected Timing Feel | Morning Clarity Guidance | Provider Will Screen For |
|---|---|---|---|---|---|
Sleep Onset (can’t fall asleep) | Falling asleep faster; calming nervous system | Clonidine | Peak effects typically 1-3 hours; take 60-90 mins before bed | Clear mornings with consistent timing; adjust 15-30 min earlier if clarity <7 | Blood pressure history; tendency toward dizziness |
Sleep Maintenance (wake up during night) | Staying asleep; deeper sleep stages | Trazodone | Works in 30-60 minutes; reduces nighttime awakenings | Most report clear mornings; timing adjustments resolve any heaviness | Other medications; heart health history |
Racing Thoughts / Anxiety | Quieting mental activation | Hydroxyzine | Typically sedating within 30-60 minutes | Maintain consistent timing window for best morning clarity | Pregnancy/breastfeeding; other sedating medications |
Morning Clarity Score (1-10 Scale):
- 10 = Clear, normal energy and focus within 15 minutes of waking
- 7-9 = Workable, minor heaviness that clears quickly
- 4-6 = Noticeable fog; timing/interactions need review
- 1-3 = Significant impairment; contact clinician promptly
Quick Troubleshooting Flow:
If your Morning Clarity Score is below 7 for three consecutive mornings:
- First, review your timing window and avoid-list compliance (alcohol, late caffeine, screen exposure)
- Work with your clinician to shift your dose 15-30 minutes earlier in the evening
- If grogginess persists after timing adjustments, your clinician may consider dose or medication changes
Most morning fog stems from timing and evening habits—not the medication itself—and small adjustments often resolve it quickly.
For detailed medication information including how they work, dosing ranges, and what to expect, see the medication selection page and our comprehensive treatments offered guide.
Step 3 — Timing Windows That Protect Tomorrow
Here’s the insight most people discover too late: morning clarity depends more on when you take your medication than on which medication you take.
The Bedtime-Anchored Dosing Rule
Consistent timing windows deliver clear mornings more reliably than dose adjustments. Pick a 30-60 minute window aligned to your target bedtime and stick to it. Taking your medication at 10:15 PM on Monday, 11:45 PM on Tuesday, and 9:30 PM on Wednesday creates unpredictable morning clarity—even if the dose stays the same.
Your clinician will help you establish your initial timing window. During your first week, you’ll track a simple morning clarity score (1-10 scale, where 10 is “felt completely clear and alert within 15 minutes of waking”). If your clarity score drops below 7 for three consecutive mornings, your clinician may suggest moving your dose 15-30 minutes earlier to give your body more processing time before your alarm.
Why Consistency Matters More Than You Think
Your body metabolizes these medications based on their specific half-life. When you take your dose at the same time each night, you align the medication’s peak levels with your natural circadian drop in alertness. Consistent timing prevents ‘dose creep,’ ensuring the medication has been sufficiently cleared from your system by the time your alarm rings.
Step 4 — What to Avoid (So the Medication Can Actually Work)
The what-to-avoid checklist protects treatment effectiveness and morning clarity. These aren’t arbitrary rules—each item on this list either blocks your medication’s sleep-promoting effects or extends its active time in your system.
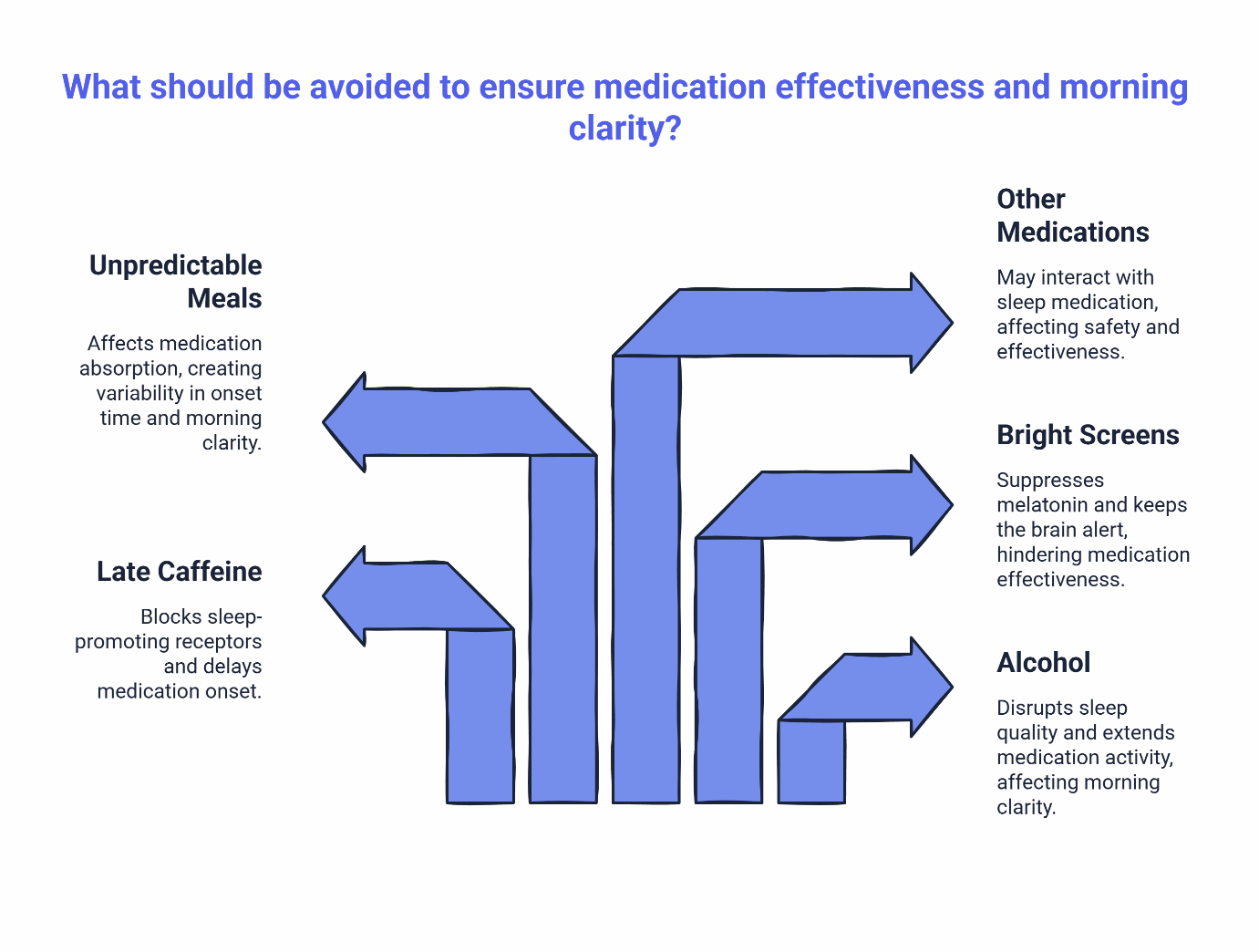
The Essential Evening Guidelines:
Alcohol — Skip alcohol within 4-6 hours of your dose. It disrupts sleep quality and can extend how long the medication stays active, affecting morning clarity.
Late Caffeine — Cut caffeine by 2 PM. Caffeine blocks adenosine receptors that promote sleep, working against your medication’s effects even 6-8 hours after consumption. Clinical pharmacokinetics confirm that half of a caffeine dose remains in your system up to 5 hours later, delaying the onset of sleep aids.
Bright Screens / Blue Light — Reduce device exposure 1-2 hours before bedtime when possible. Screen light suppresses melatonin production and keeps your brain alert, as documented by Harvard Health research on blue light exposure, making it harder for your medication to work effectively.
Unpredictable Meal Timing — Large, heavy meals close to bedtime or an empty stomach can both affect how quickly your medication is absorbed, creating variability in onset time and morning clarity.
Other Medications — Always inform your clinician about all medications, supplements, and over-the-counter products you take. They’ll ensure your sleep medication works safely with everything else.
For complete guidance on optimizing your evening routine while taking sleep medication, see Non-Controlled Sleep Medications: What to Avoid to Prevent Morning Grogginess.
Step 5 — The First 7 Nights Playbook (Installing Sleep Auto-Pilot)
The first week is your calibration period. You’re not just taking a medication—you’re installing a new routine that your body will learn to anticipate. Here’s your night-by-night framework:
Your First-Week Routine:
- Same Bedtime Cue (Every Night) — Choose a simple trigger 15 minutes before your dose: turning off devices, changing into sleep clothes, dimming lights. Your brain will start associating this cue with the upcoming medication and sleep transition.
- Same Timing Window (±15 Minutes Maximum) — Take your medication within the same 30-minute window every night. Set a phone reminder if needed. Consistency here determines your morning clarity more than any other factor.
- Track Your Morning Clarity Score (1-10 Scale) — Within 15 minutes of waking, rate your alertness. Be honest: 1 = “felt like moving through fog,” 10 = “felt completely sharp and ready.” Write it down or note it in your phone. Three consecutive scores below 7 signal it’s time to message your clinician about a timing adjustment.
- Follow Your Avoid List (No Exceptions) — The first week isn’t the time to test boundaries. Skip alcohol entirely, cut caffeine by 2 PM, and keep screens off for 90 minutes before your dose.
- Note Any Mild Effects — Dry mouth, slight dizziness when standing, or feeling unusually relaxed are common during the first 2-3 nights as your body adjusts. These typically fade. Jot them down so you can report patterns to your clinician, not just isolated incidents.
- Know Your Outreach Thresholds — Message your clinician if you experience anything concerning or if morning grogginess persists beyond a few days despite timing adjustments.
- Stay Patient for 5-7 Nights — Your body needs several consistent cycles to fully adapt. Many people feel a noticeable improvement by night 3, but full stabilization often takes a week.
By night 7, you’ll have enough data to evaluate the pattern-fit and make informed timing adjustments with your clinician if needed.
This supervised medication approach works best when paired with solid sleep fundamentals. Think of it as a “paired path”—the medication provides reliable sleep onset while you strengthen the habits that sustain good sleep long-term. For context on how medication-supported plans compare to habit-focused approaches alone, see Non-Controlled Sleep Medications vs. Sleep Hygiene Alone.
Step 6 — What to Expect in the First Week
Starting a new sleep medication often comes with short-term adjustment effects that resolve as your body adapts. Knowing what’s normal helps you feel confident during the first few nights.
Common Experiences (Usually Resolve in 3-5 Days):
- Dry mouth in the morning
- Mild drowsiness when first waking (typically clears within 30-60 minutes)
- Feeling unusually relaxed or calm in the evening
- Slight lightheadedness when standing up quickly in the first hour after waking
The Timing-First Approach:
Before assuming you need a different medication or dose, work with your clinician to try a timing adjustment. Shifting your dose 15-30 minutes earlier in the evening resolves most mild morning drowsiness without requiring a prescription change. This approach—adjusting the clock before adjusting the medication—is often faster and more effective.
When to Contact Your Clinician:
- Morning drowsiness that persists beyond the first hour or doesn’t improve after timing adjustments
- Any symptoms that concern you or affect your daily activities
- Questions about how your medication is working
For detailed information about what to expect with specific medications, see Non-Controlled Sleep Medications Side Effects: A Plain-English Guide.
For medication-specific information from authoritative sources:
The Key Principle: Your clinician wants to hear from you. Reaching out early helps fine-tune your treatment faster and ensures the best possible outcomes.
Step 7 — Travel & DST: Keeping the System Working
Once you’ve established your routine, travel and daylight saving time shifts can disrupt it. The core principle stays the same: maintain your timing window relative to your target bedtime in your current location, not the clock time you used at home.
Quick Travel Guidance:
- Shift your dosing time gradually if crossing multiple time zones (15-30 minutes per day)
- Maintain your avoid-list discipline even when routines are disrupted
- Pack your medication in carry-on luggage to ensure access
- Keep your morning clarity tracking going—it’s your best feedback loop
Daylight Saving Time Transitions:
- Spring forward: Take your dose 15-30 minutes earlier for 2-3 nights to ease into the time change
- Fall back: Gradually shift your dose 15-30 minutes later over 2-3 nights
For comprehensive planning tools and zone-specific strategies, see Non-Controlled Sleep Medications & Travel: Adjusting for Time Zones and DST.
Step 8 — How Supervised Online Sleep Care Works (SleepScriptMD)
If you’re ready to explore a clinician-guided plan with safe, non-addictive prescription options, here’s how the SleepScriptMD process works.
Two Pathways for Care:
Asynchronous AI-Assisted Care — Complete an online assessment at your convenience. An AI-assisted system organizes your responses, but a licensed physician reviews and approves every prescription decision. Most patients receive a treatment recommendation within hours. Note: If a medication affecting blood pressure (like Clonidine) is considered, you may be asked to provide a recent BP reading to ensure safety.
This pathway works well for straightforward cases without complex medical histories.
Cost: $45 for 30 days or $120 for 90 days (medication cost paid separately at your pharmacy)
Virtual Session — Schedule a live video consultation (typically available within 5 days) with a licensed provider for a more hands-on evaluation. This pathway is better for patients with moderate medical concerns or those already taking sleep medications that aren’t working. Some states require a video visit due to local telehealth regulations.
Cost: $110 for a 25-minute intake (includes 30-day prescription if appropriate; medication cost paid separately at your pharmacy)
Both pathways include the same physician oversight, safety screening, and follow-up support. The difference is the format—asynchronous text-based review versus live conversation.
The Eligibility Gate and Safety Screens:
Before prescribing, clinicians verify:
- You’re between 18-65 years old
- You don’t have major medical, mental health, or substance use conditions that make sleep medications unsuitable
- You’re not pregnant and not planning pregnancy
- If you snore, gasp, or stop breathing during sleep, you’ll need an at-home sleep test before treatment begins (medication isn’t prescribed until test results are reviewed)
What We Prescribe: We focus exclusively on safe, non-controlled prescription sleep medications like trazodone, hydroxyzine, and clonidine. We do not prescribe benzodiazepines (like Xanax or Valium) or Z-drugs (like Ambien or Lunesta) due to their dependency risks.
For detailed pricing, process flow, and state-specific requirements, see:
All care is HIPAA-compliant, and prescriptions are sent electronically to your preferred pharmacy.
FAQs
Are these medications addictive?
No. Non-controlled sleep medications like clonidine, trazodone, and hydroxyzine don’t carry the dependency risks of controlled substances. They work through different mechanisms—calming the nervous system, blocking histamine, or enhancing deep sleep—without creating the tolerance or withdrawal issues associated with benzodiazepines or Z-drugs. Your clinician will guide you on the right approach if you ever decide to stop.
How fast do they work?
Most non-controlled sleep medications begin working within 15-60 minutes, depending on the specific medication and your pattern-fit. Clonidine and hydroxyzine typically show effects within 30-60 minutes, while trazodone often takes 30-60 minutes to help you fall asleep and continues working to extend deep sleep throughout the night. The key is taking your dose at the same time each night—consistency speeds up how quickly you feel the effects because your body learns the rhythm.
What if I wake up groggy?
First, check your timing window. If your morning clarity score is below 7 for three consecutive mornings, work with your clinician to shift your dose 15-30 minutes earlier. Most grogginess resolves with timing tweaks, not medication changes. Also verify you’re following your avoid list (no alcohol, cut caffeine by 2 PM, screens off 90 minutes before dose). If grogginess persists after timing adjustments, your clinician may consider a different medication or dose.
Can I drink alcohol while taking these medications?
It’s best to avoid alcohol within 4-6 hours of your dose. Alcohol can disrupt sleep quality and extend how long the medication stays active in your system, affecting morning clarity. If you want reliable sleep and clear mornings, skipping evening alcohol during treatment helps your medication work as intended.
What about caffeine?
Cut caffeine by 2 PM. Caffeine blocks adenosine receptors that promote sleep, working against your medication’s effectiveness even 6-8 hours after consumption. Late-afternoon or evening caffeine makes it harder to fall asleep and reduces sleep quality. If you need an afternoon pick-me-up, switch to decaf or herbal tea after lunch.
What about other medications I’m taking?
Always inform your clinician about all medications, supplements, and over-the-counter products you take. They’ll review everything to ensure your sleep medication works safely with your current regimen. This is a standard part of the prescribing process.
What if I need to travel or deal with daylight saving time?
Maintain your timing window relative to your target bedtime in your current location, not the clock time you used at home. For multi-time-zone travel, shift your dose gradually (15-30 minutes per day). For DST transitions, adjust by 15-30 minutes over 2-3 nights. Keep tracking your morning clarity score during transitions—it’s your feedback loop. See the travel guide for detailed zone-specific strategies.
When is this not just insomnia?
Some sleep problems require in-person evaluation by a specialist before starting medication. Contact a local sleep specialist or your primary care provider if you experience:
- Falling asleep unexpectedly during the day (while talking, driving, or during routine activities)
- Sudden muscle weakness triggered by strong emotions (laughing, anger, excitement)
- Feeling paralyzed when falling asleep or waking up
- Acting out dreams physically during sleep (yelling, kicking, punching)
- Uncontrollable urges to move your legs at night or while resting
These symptoms may indicate conditions like narcolepsy, REM sleep behavior disorder, or restless legs syndrome, which need different evaluation and treatment approaches than standard insomnia.
Your Path to Predictable Sleep
You’ve spent enough nights doing the math at 2 AM. The pattern-fit approach replaces that calculation with a system: identify your insomnia pattern, match it to the right safe, non-addictive medication under clinician supervision, establish a consistent timing window, follow your avoid list, and track your morning clarity score to fine-tune during the first week.
This isn’t about “knocking yourself out.” It’s about installing sleep auto-pilot—a predictable routine that works with your body’s natural systems, protects your morning performance, and gives you back the nights you’ve been losing to insomnia.
Ready to Start Your Sleep Treatment?
Take the 6 Second Sleep Check for a fast baseline, or use the Sleep Clarity Quiz to understand your pattern better. For a comprehensive evaluation, try the Deep Sleep Profiler.
When you’re ready for a clinician-guided plan with safe, non-addictive prescription sleep aids, get started with our simple eligibility check and see how our supervised care process works:
Or explore pricing options to find the pathway that fits your needs.
Disclaimer: This content is for educational purposes only and is not medical advice. Do not start, stop, or change any medication without speaking with a licensed clinician. If you think you may have a different sleep disorder or a medical emergency, seek in-person care right away.
Our Editorial Process
Our expert team uses AI tools to help organize and structure our initial drafts. Every piece is then extensively rewritten, fact-checked, and enriched with first-hand insights and experiences by expert humans on our Insights Team to ensure accuracy and clarity.
About the SleepScriptMD Insights Team:
The SleepScriptMD Insights Team is our dedicated engine for synthesizing complex topics into clear, helpful guides. While our content is thoroughly reviewed for clarity and accuracy, it is for informational purposes and should not replace professional advice.
